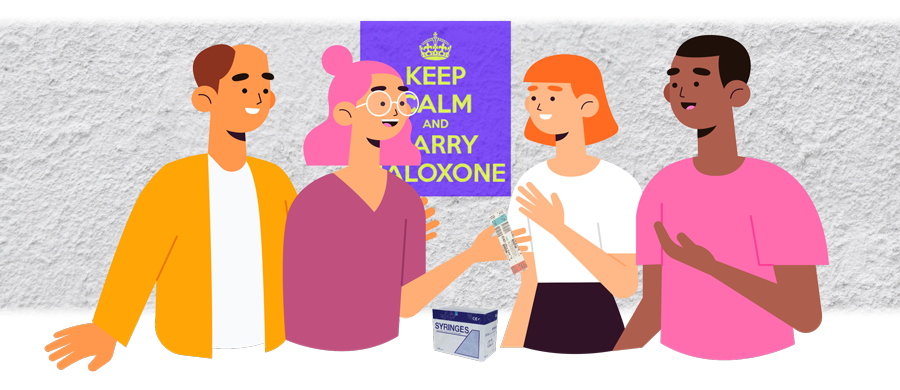
Among its other services, Hepatitis SA runs four Clean Needle Program (CNP) sites in Adelaide, at Hackney, Noarlunga, Port Adelaide, and Salisbury. Our CNP peer educators also attend rostered sessions at other sites at various times during the week.
In late 2019, we celebrated this program’s fifth successful year, which would have been impossible without the hard work and dedication of our peer educators, who have personal experience and knowledge of injecting drug use and also have up-to-date knowledge on hepatitis B, hepatitis C and other blood-borne viruses.
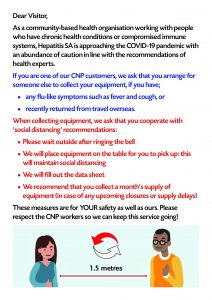
Even with the COVID-19 outbreak and mass closure of services, Hepatitis SA’s peers continue to offer CNP services, with extra physical distancing arrangements in place for the safety of both clients and workers.
We asked some of Hepatitis SA’s peer educators to reflect on how they came to the job, and what rewards they find in it.
What first made you want to be a peer worker at Hepatitis SA?
MARGIE: I became a peer worker because I wanted to help drug users get the correct information about how to use drugs and do the least amount of damage to your body and mind while doing it.
PENNI: I first wanted to be a peer worker at Hep SA when they adopted CNP management—due to the focus on blood-borne viruses, this made sense. I was already familiar with the roles of CNP operator and peer educator from previous work in the field, and really enjoyed and felt fulfilled in the position, and felt an affinity for the work and the clients. I wanted to continue my existing employment as a CNP peer along with my existing part-time peer educator role with HepSA, so I was fortunate that I could perform both roles on a part time basis, plus the subject matter overlapped, permitting me to engage in both CNP and HCV peer education work. I could bring skills from either specific role to help the other.

MARGIE: I started using in the 1980s, when the only information came from other users. There were no CNPs, no Google, so you learned from others. We bought equipment from medical supplies shops. We bought glass barrels called Blue Ladies, and boxes of tips. There was no swabbing that I can remember, and we used the tips over and over until they wouldn’t push through the skin anymore. We shared everything, though we did rinse the equipment a lot in between each use. As I owned a Blue Lady I got to go first—a big plus.
When I moved to Sydney there was one chemist to get equipment from, in King’s Cross. Police sat outside taking photos of everybody going in and out, so we would go as little as possible. We all shared equipment. Nearly everybody I knew had what was then called Hep Non-A Non-B, which we now know is hepatitis C. We had no idea you could get different strains—they didn’t have a name for it or any information. Then AIDS hit and sharing became a game of Russian roulette. Many didn’t win.
Then in 1986 the first needle exchange—that’s what we called them—came in. It was a life-changer. Not only could you get new equipment, you could get advice and information. If I remember correctly it was in an old police station! At that time I asked if I could volunteer there because I thought it was an amazing service. They didn’t have peers at the time so I was given the job of making up 10-packs. I didn’t last that long as I was put in a room alone and, to be honest, I got bored.
Life moved on and I didn’t really think about working in CNPs or being involved until I came to South Australia. I was told about SAVIVE and started volunteering there. It was great to be around people that felt the same about treating drug users with respect and offering as much information as I could to keep them safe. When a job came up at Hep SA as a peer educator, I jumped at the chance to apply.
SUE: I had been a peer worker for about 10 years when the AIDS Council, which used to fund the SAVIVE and SIN injecting drug programs, closed down, so I came to work for Hepatitis SA.
Being a peer worker fulfilled me with work that I found myself good at. I have learned to listen, and to give the clients some referral advice in the areas that might help them. However, I cannot do the job for them, and I believe we need more advocates to assist people lost in their own depression or lifestyle choices. We peers have all been around for a number of years now, so we have all have a great rapport and trust with our clients.