A Story of Mixed Success
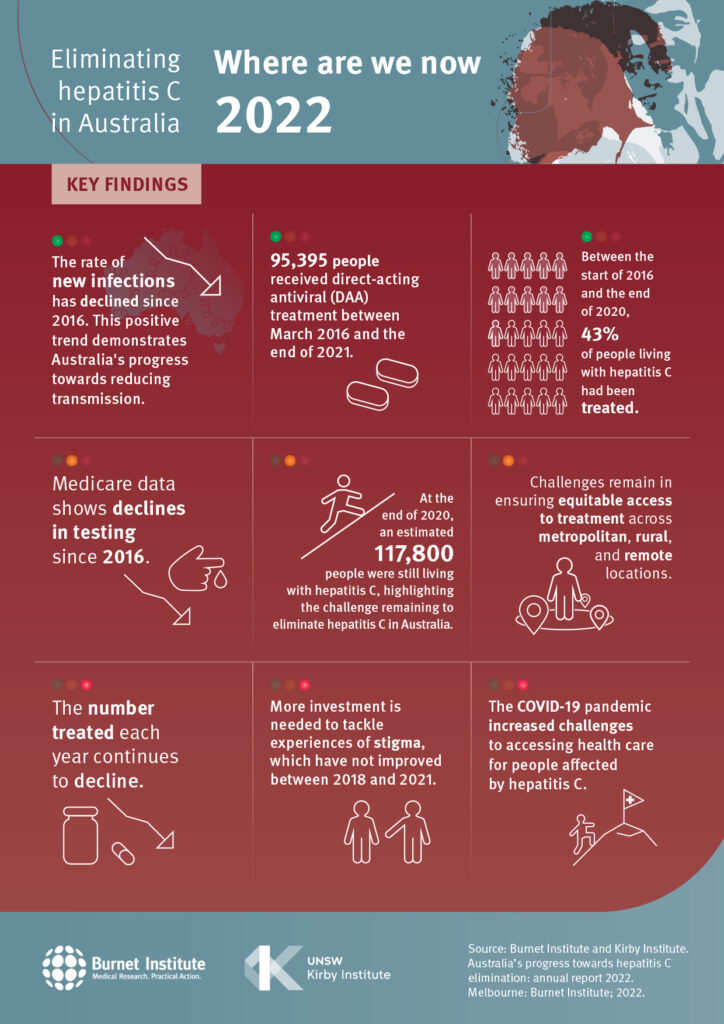
The newly released 2022 annual report from the Burnet and Kirby institutes, Australia’s Progress Towards Hepatitis C Elimination, has a story of mixed success to tell.
Unrestricted access to direct-acting antivirals (DAAs) through public subsidy since March 2016 means there is a real opportunity to reach the official government target of eliminating hepatitis C as a public health threat in Australia by 2030.
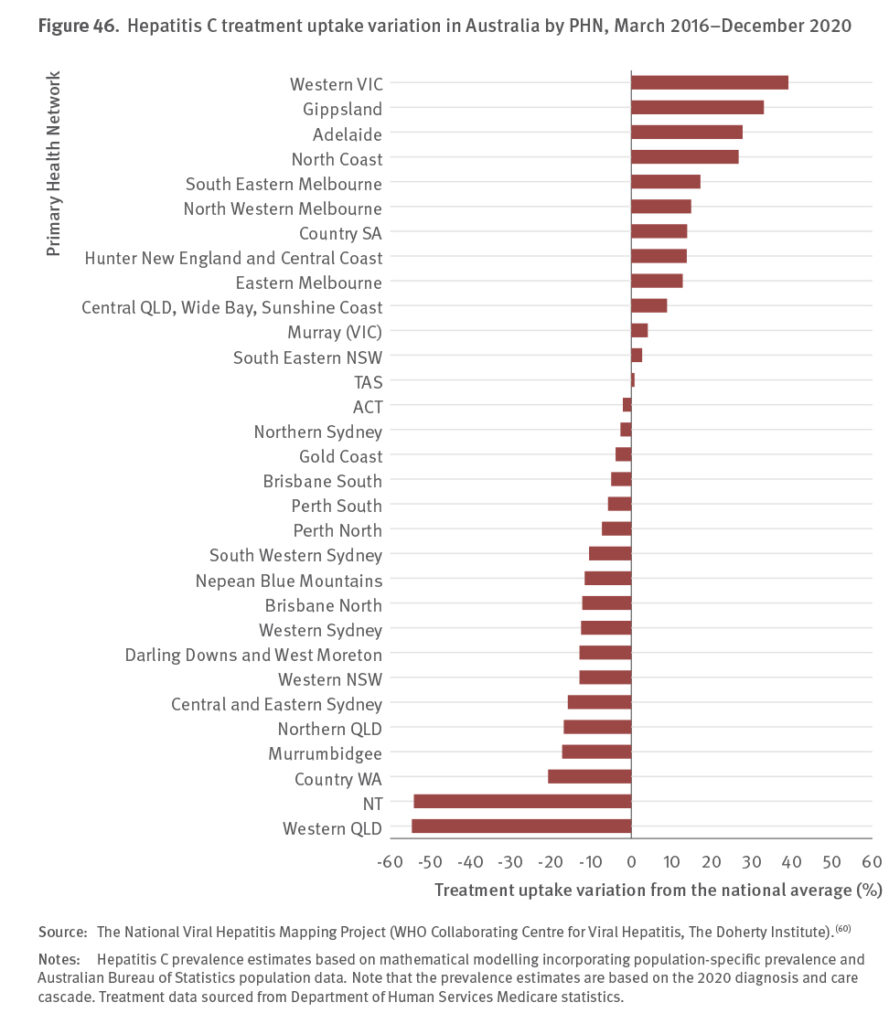
However, at the end of 2020, an estimated 47% of people living with hepatitis C were yet to be treated, representing 117,800 people living with chronic hepatitis. It is clear from data collated in this year’s report that declines in testing and treatment are substantial and ongoing. Without a reinvigoration of efforts to increase diagnosis, Australia will definitely not achieve its elimination goals.
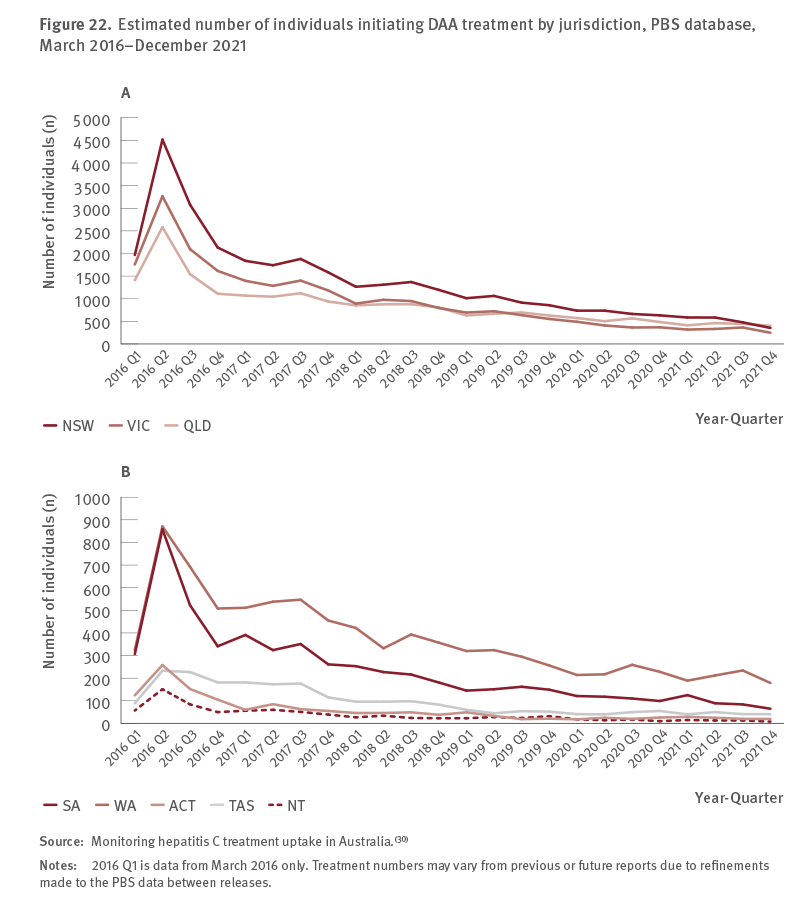
March 2016–December 2021
To understand progress towards hepatitis C elimination, monitoring trends in data to assess the impact of these components is required, from measurement of new infections, counts of people tested and treated, and people receiving hepatitis C‑related liver transplants, through to projections based on mathematical modelling. This is the fourth national report on progress towards hepatitis C elimination in Australia. It brings together national data from across the sector, to give an overview on progress towards eliminating hepatitis C in Australia. This report also highlights gaps in our knowledge and informs future directions in Australia’s hepatitis C elimination response.

Australia has made considerable progress towards elimination in recent years with 95,395 people initiating DAA treatment between March 2016 and the end of 2021. Where available, the data show that numbers/rates of current infections have declined, particularly among the priority population of people who inject drugs and among HIV‑positive men who have sex with men.
Of note, there has been a significant and increasing contribution of prison‑based hepatitis services in progressing Australia’s elimination goals. In 2021, DAA treatment initiations in prison‑based hepatitis services represented 41% of the total national DAA treatment initiations, an increase from 2019 (30%) and 2020 (37%). These data reflect the ongoing importance of supporting the justice sector to eliminate hepatitis C and underscore the crucial role prison hepatitis services play in reaching people at risk of hepatitis C and Australia achieving its elimination goals.
Despite these successes over the past six years, that still leaves us to face the uncomfortable figure of 117,800 people living with chronic hepatitis C, highlighting the considerable challenge that remains to eliminate hepatitis C in Australia.
Levels of hepatitis C testing, and therefore diagnosis and treatment have declined. While this decrease in the number of people living with hepatitis C who have been tested and was observed prior to the COVID‑19 pandemic, the pandemic definitely exacerbated the decline and continues to create additional challenges to accessing health care for people affected by hepatitis C.
To ensure elimination goals are met health promotion campaigns are needed to ensure key risk populations are aware that treatment and retreatment is available to them and to encourage them to engage in care.
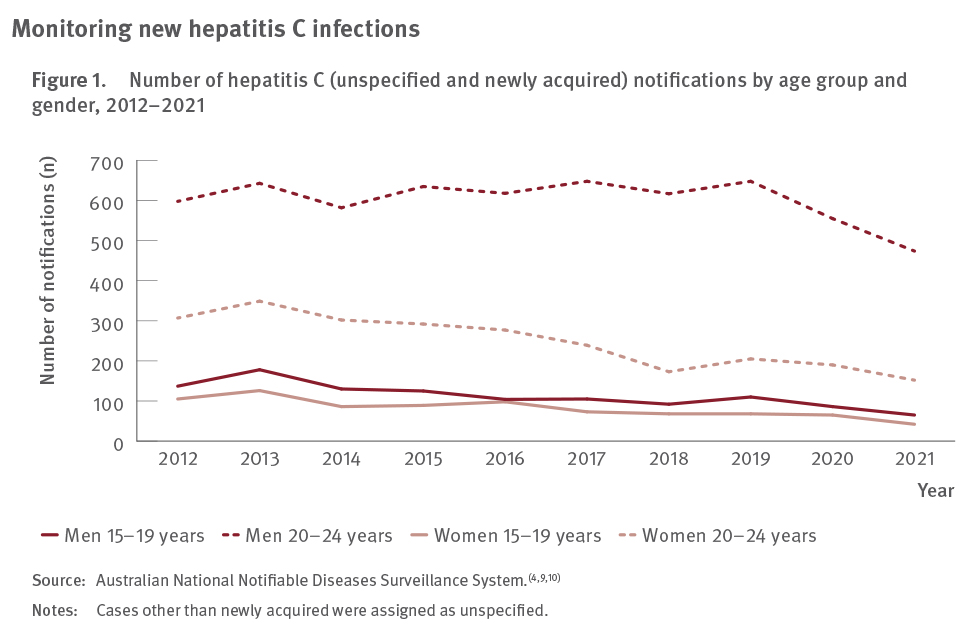
gender, 2012–2021
Considerable effort and investment are also needed to support the provision of accessible, simplified, and convenient models of testing and treatment, to ensure people living with or at risk of hepatitis C access testing, are retained in care, and complete treatment in a timely fashion.
This may include novel models of care such as point‑of‑care testing, of the sort Hepatitis SA is heavily involved in, as well as peer‑led models of care, testing and treatment in non‑traditional settings such as pharmacies, and expanding drug treatment programs to include hepatitis C care.
Expanding models of care also requires supporting the relevant workforce through education and skill development.
There also needs to be ongoing investment in the prevention of new infections and reinfection through harm minimisation, including in prisons.
Importantly, this report highlights that stigma and discrimination towards people at risk of and living with hepatitis C remains prevalent. Interventions to reduce stigma in the community and health care settings will be necessary to increase engagement with hepatitis C testing and treatment services and continue progress towards hepatitis C elimination.
2030 is close, and more action is needed now.
THE COVID-19 FACTOR
To examine how COVID‑19 related restrictions changed uptake of HCV antibody and HCV RNA testing, data from 11 ACCESS clinics located in Victoria which specialise in the care of people who inject drugs were included in a careful analysis.
Data from all services during the 125 weeks between 1st January 2019 and 25th May 2021 were included, thus including a year of data from before the pandemic, as well as more than a year of data once the pandemic began.
Pre‑COVID, an average of 80.6 HCV antibody and 25.7 HCV RNA tests were performed each week (note that a declining trend was observed prior to COVID‑19‑related lockdowns). After the first lockdown in Victoria (April 2020), there was an immediate drop of 23.2 HCV antibody tests and 8.6 HCV RNA tests per week (equivalent to a 30.9% and 46.0% drop, respectively).
After the second Victorian lockdown (July 2020), there was an immediate drop of 17.2 HCV antibody tests and 4.6 HCV RNA tests per week (equivalent to a 26.2% and 33.3% drop, respectively).
Some recovery in HCV antibody testing in the months following the lockdowns was observed, but the average level of HCV antibody testing had not returned to pre–pandemic levels by the end of May 2021.
It is important to note that Victoria’s lockdowns were the most severe for an state in Australia.