The Viral Hepatitis Mapping Project looks at geographic variations in the prevalence of viral hepatitis across Australia, as well as access to care, to identify priority areas for response. It is a joint initiative of the WHO Collaborating Centre for Viral Hepatitis Epidemiology, The Doherty Institute and ASHM, funded by the Australian Government Department of Health and Aged Care.
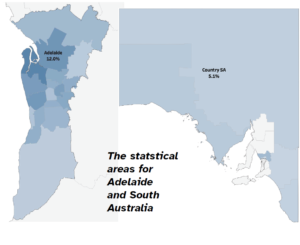
The project is especially useful because it divides the country up into small areas (sometimes called statistical areas or SAs), meaning that it can be used to pinpoint exactly where and how easily people are being diagnosed and treated across the country. Localised health care and access to treatment for hepatitis B and C is a key objective of recent healthcare reform in Australia and enhancing access to treatment and care is a priority action in both the National Hepatitis B Strategy 2018-22 and the National Hepatitis C Strategy 2018-22.
The Project’s national report on hepatitis B for 2021 has just been published, and it shows some interesting and concerning trends (the report on hepatitis C is forthcoming).
PREVALENCE
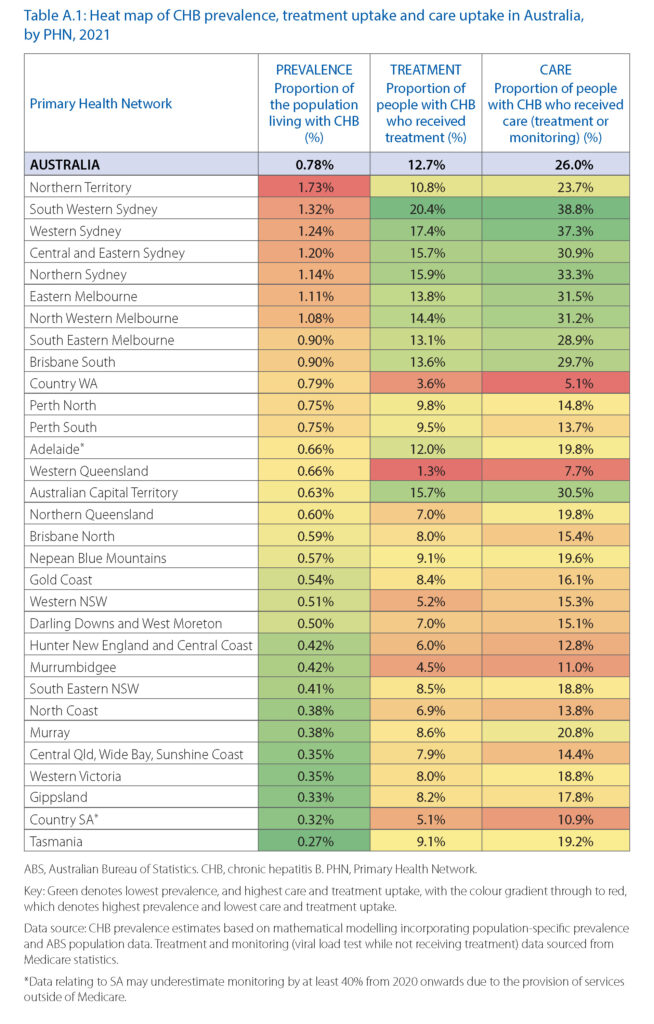
An estimated 200,385 people were living with chronic hepatitis B (CHB) in Australia in 2021, representing 0.78% of the total population.
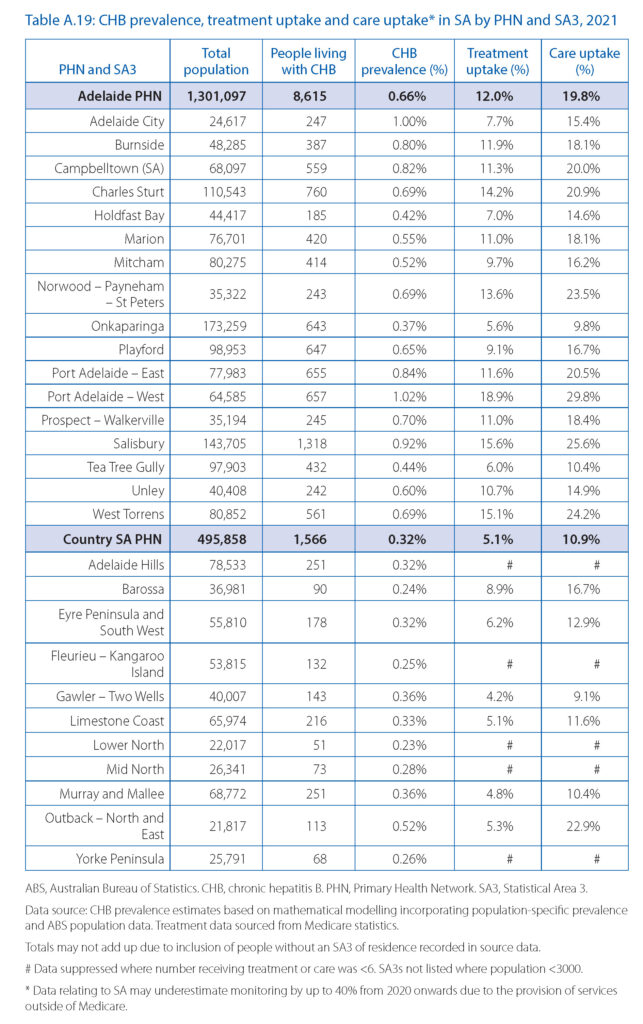
The highest rates, by a significant margin, were found in the Northern Territory (1.73%, more than twice the national average), while Adelaide and Country SA were below the average (with 0.66% and 0.32% respectively).
TREATMENT
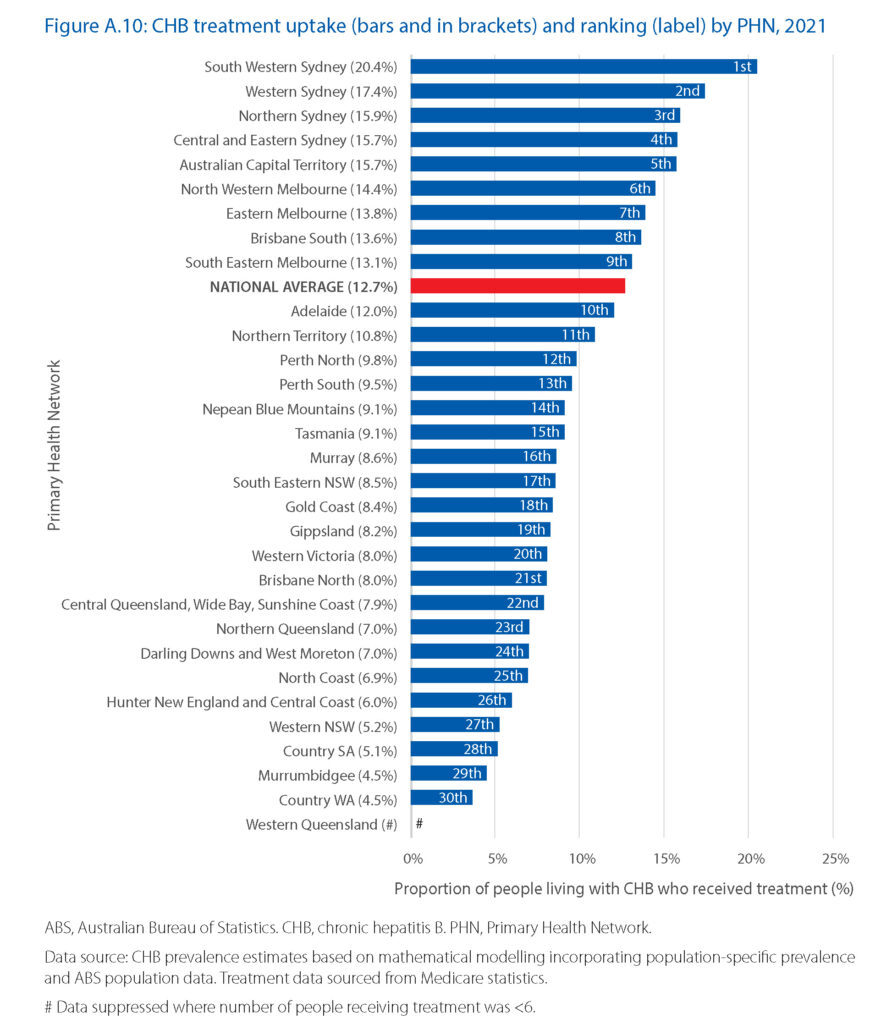
Some people living with hepatitis B require antiviral therapy to prevent disease progression. Nationally, treatment uptake for chronic hepatitis B in 2021 was 12.7%, which is significantly short of the target of 20% set by the National Hepatitis B Strategy 2018–2022. Worryingly, although the number of people receiving treatment has increased over time, the rate of increase has reduced in recent years.
Treatment uptake was highest in Public Health Networks (PHNs) in Sydney, Melbourne, and Brisbane, as well as in the Australian Capital Territory.
Only 13 of the statistical areas (4.4% of those reported) had already reached the 2022 treatment uptake target of 20%.
General practitioner (GP) prescribing for hepatitis B treatment was stable in 2021, and 22.2% of people treated for it in 2020 had a GP prescribe at least one of their prescriptions.
CARE
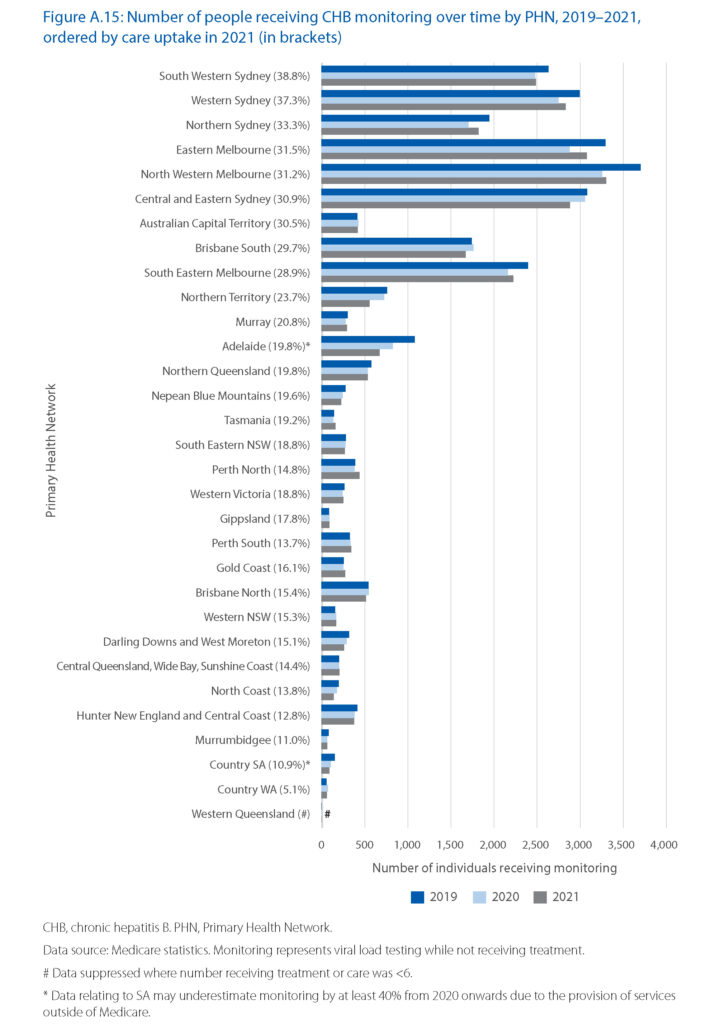
All people living with hepatitis B should be engaged in care. Nationally, engagement in care (either undergoing treatment or regular monitoring of disease progression) in 2021 was 26.0%, which is sadly only just over half the National Strategy 2018–2022 target of 50% by 2022.
As with treatment uptake, care uptake was highest in PHNs in Sydney, Melbourne, Brisbane and Australian Capital Territory. Only three statistical areas had already reached the National Strategy 2018–2022 care uptake target of 50% by 2022. These were in the Northern Territory (East Arnhem), Northern Queensland (Far North) and Brisbane South.
Overall, the number of people engaged in monitoring (those who received a viral load test while not receiving antiviral treatment) reduced in 2020 and in 2021, impeding progress toward the care uptake target. GPs provided almost half of all monitoring tests in 2021.
IMMUNISATION
Hepatitis B immunisation is recommended for all infants born in Australia. Further, there are also publicly funded immunisation programs to ensure certain higher risk groups are also able to access hepatitis B vaccine.
Even though in previous years the National Strategy 2018–2022 target of infant immunisation against hepatitis B, a rate of 95%, has been met, in 2021 the national rate declined to 94.6%.
Coverage was even lower among Aboriginal and Torres Strait Islander children (91.8%), and this also declined between 2020 and 2021.
The 95% coverage target was met in 16 of Australia’s 31 PHNs for all children, and in eight PHNs for Aboriginal and Torres Strait Islander children.
TESTING TRENDS
Maintaining high testing rates among all populations at risk is critical to ensure people living with hepatitis B are quickly diagnosed and linked to care. Nationally, the number of hepatitis serology tests occurring through Medicare reduced in 2020, and this decline has continued through the end of 2022, resulting in an estimated 1.3 million fewer serology tests over this time period.
Although the rate of decline varied, between 2019 and 2022 it took place in all states and territories.
CARE UPTAKE IN SOUTH AUSTRALIA
Treatment uptake for hepatitis B in SA during 2021 was measured at 10.9%, notably lower than the national average of 12.7%. SA ranked in fourth place for treatment uptake out of the eight states and territories.
As you might expect, given ease of access, treatment uptake was highest in Adelaide and lower in more remote regions. In the Adelaide PHN it was 12%, and an impressive 18.9% in the Port Adelaide – West statistical area. Though this was still below the 20% target from the national strategy, if the trends in the number of people receiving treatment in this area continue, it is projected to have reached the 20% National Strategy treatment uptake target in 2022.
Treatment uptake was also above the national average in the Salisbury (15.6%), Charles Sturt (14.2%) and Norwood – Payneham – St Peters (13.6%) statistical areas. However, there was a decline in the rate of people receiving treatment in the Mitcham, Playford and Unley statistical areas.
Assessing variation in treatment uptake within Country SA is difficult, as most statistical areas in the region have a small population, leading to high uncertainty within the data. However, the available data does not suggest substantial variation in uptake within the PHN. The number of people receiving treatment in this PHN increased at a similar rate to the national trend during 2019–2021.