Hepatitis SA Education Coordinator, Jenny Grant, was at the 14th Viral Hepatitis Conference in Darwin, as delegate and presenter. She shares her take on the three-day event.
The 14th Australasian Viral Hepatitis Conference for 2024 was held in early August on the beautiful lands of the Larrakia People in Darwin. This year’s conference had a different feel to it: much as in the classic Australian movie The Castle, it was the vibe, and this was commented on by numerous people I spoke with.
There were presentations from across Australia and the region covering all aspects of viral hepatitis. On the first morning, I attended a pre-conference meeting held by the Kirby Institute on ‘Implementation Process Mapping of Hepatitis C Point-of-Care Testing’. Participants shared their experiences and the creative ways they are engaging with the community to increase testing, including the use of incentives other than cash (like linking up with the courts to have people’s fines reduced when they are engaging with their service, or providing top-ups to bus cards).
…creative and passionate people are in coming up with new ways to reach the community and go to where they are.
There are also a lot of mobile clinics getting around Australia, ranging from fully decked-out vans to the back of someone’s Camry. One thing that definitely came out of this meeting was how creative and passionate people are in coming up with new ways to reach the community, and in going to where they are. The Kirby Institute will pull together all of the discussions which will then allow other services to implement new strategies.
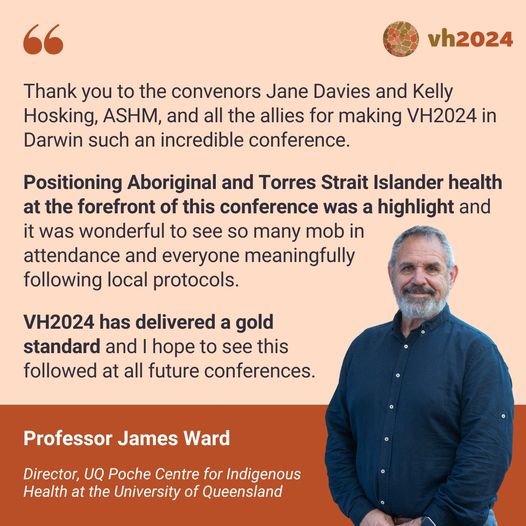
When the conference officially commenced, we were welcomed to the beautiful lands of the Larrakia People by Yvonne Odegaard, whose clan group is Saltwater Crocodile, Dangalabba, a proud Saltwater woman and traditional owner. Following Yvonne was the Convenor’s Welcome; Associate Professor Jane Davies talked about our need to work together to build connections, foster partnerships and collaborate to reach the 2030 viral hepatitis elimination goals.

Afterwards I attended the session on implementing the national hepatitis strategies. There was talk of the money being invested in viral hepatitis through the national budget, but how it wasn’t enough. Some good news, though, is that there is mention of implementing needle and syringe programs in custodial settings, and implementing universal hepatitis B screening for all adults born before the year 2000 whose hepatitis B status is unknown.
The panel was asked what they thought was the most important items in the national strategies, and the consensus was that ending stigma and increasing investment for community-based organisations to increase their amazing work so that decisions on whether, say, they could renew their $350 Survey Monkey subscription didn’t need to cause a financial crisis.
… there is mention of implementing needle and syringe programs in custodial settings, and … hepatitis B universal screening for all adults born before the year 2000.
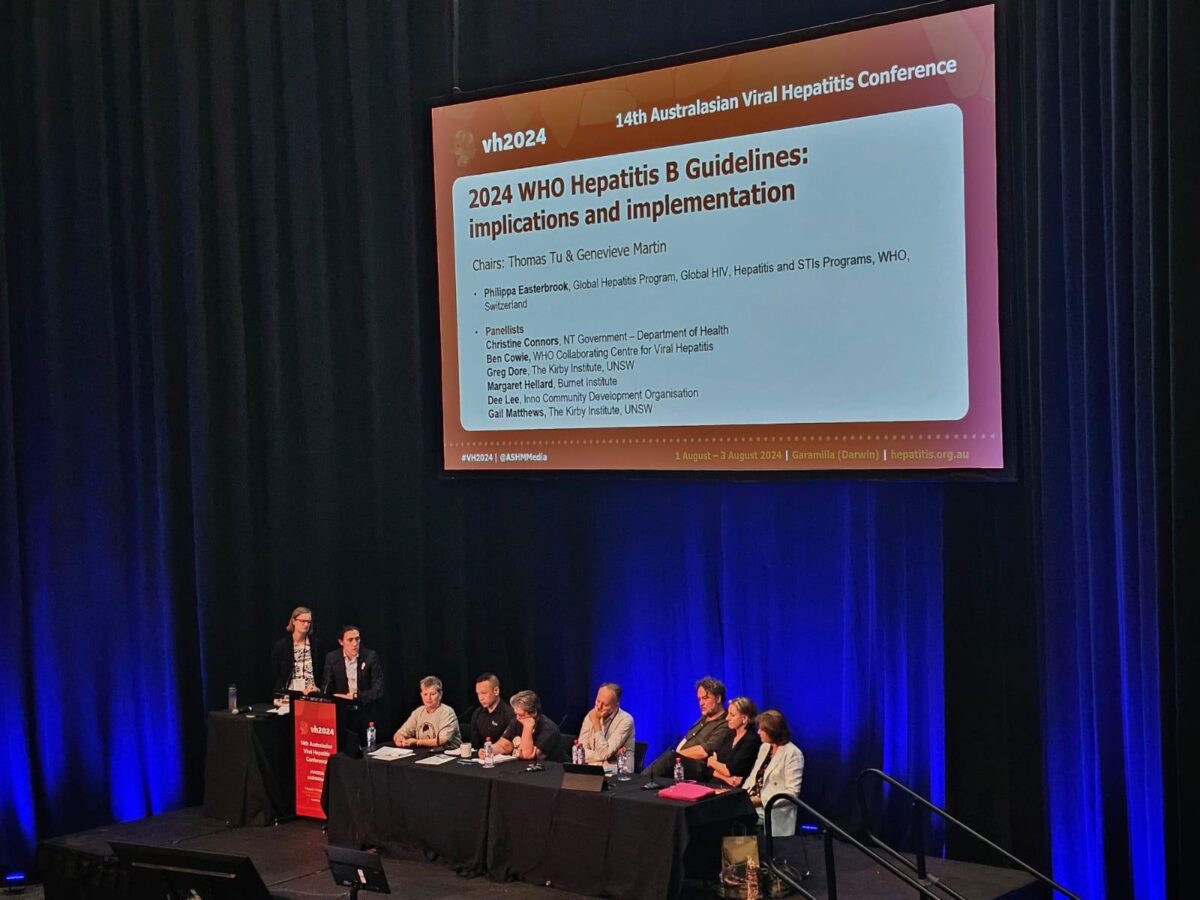
The morning of day two also had a focus on what needs to be done to reach our elimination targets, and began with Professor Ed Gane from the University of Aukland discussing the Māori people of New Zealand and the great success of the New Zealand program in the pursuit of elimination of hepatitis B. He talked about the new, simplified guidelines New Zealand has, and—as we are not on track to eliminate hepatitis B in any country—we need to screen whole populations. However, this will put immense burdens on health care systems as we find those undiagnosed patients. We should also consider treating everyone living with hepatitis B who is over the age of 30, as suppressing the virus will reduce liver cancer incidence.
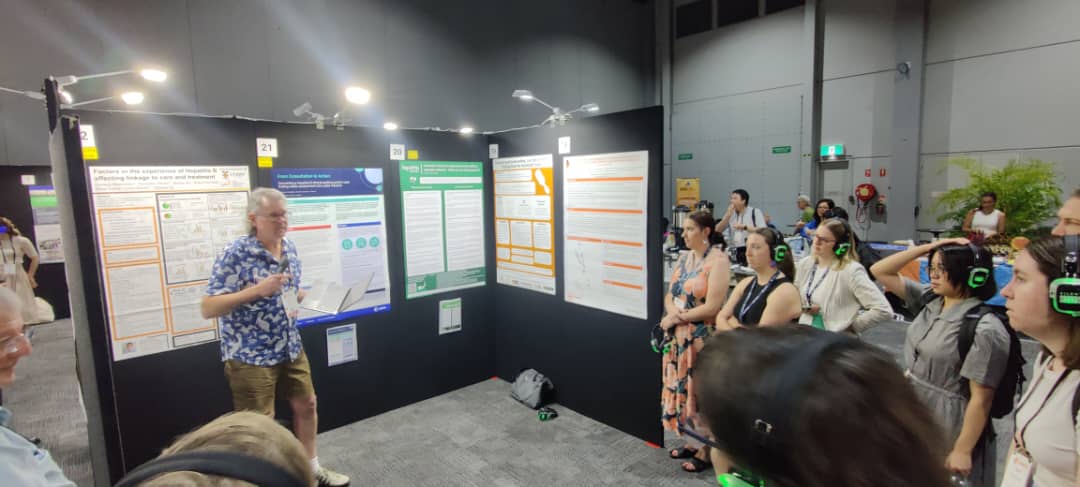
Tabletop Presentations – think ‘speed dating’
Afterwards I attended a new format of tabletop presentations: think ‘speed dating’ where there are 6 tables, 6 presenters, 10 people per table, and every 10 minutes the presenter moves to the next table and gives their presentation again. I really enjoyed this format, and look forward to participating in them again.
The first presentation was from Derbarl Yerrigan Health Service workers Jessamy, Lakhbinder, and Cameron, who discussed how their service is working to optimise the management of hepatitis B through utilising ‘Communicare’, a patient record system, to analyse data, create clinical items, and manage recalls for patients living with hepatitis B, as well as partnering with a tertiary hepatology team. Through this audit, they were looking to identify patients with chronic hepatitis B, past hepatitis B infection, isolated anti-HBc, non-immunity to hepatitis B, and close hepatitis B contacts. A total of 777 patients who would benefit from a review were identified. The team are prioritising 51 regular patients with chronic hepatitis B, ensuring their management is optimal as per the guidelines.
The next project that was of interest was ASHM’s ‘Beyond the C’ program and the work was presented by Adi and Grace from ASHM. This program is recruiting GP practices and funding them to perform clinical audits on their patient software system to identify individuals who may benefit from hepatitis C testing and treatment. Since the program launched in December 2022, 183 practices have submitted an expression of interest, and 60 have formally commenced the project. From these practices, approximately 990 people that require testing and or treatment have been identified.

The final presentation of interest was Lana Richardson from Hepatitis Queensland, who presented ‘Strength in Partnership’. Lana discussed how as a non-indigenous organisation, Hepatitis Queensland is very aware of the importance of cultural safety and community involvement and have implemented a number of strategies to ensure the success of their Hep Check program. Those include the inclusion of their Aboriginal and Torres Strait Islander Liaison Officer, following cultural protocols, creating meaningful connections and having continuous engagement utilising multiple modes of interaction.
The afternoon session I attended was discussing the UNSW’s project trialling a universal precautions approach to stigma reduction in health care. There were a few presentations in this session looking at how this project might work if Australia had a health system that would assume that all people who enter a health service might be fearful of being treated negatively or excluded in some way, thus creating an approach where, just as healthcare workers assume all blood and bodily fluids are potentially infectious, the same could be true for people who have experienced stigma. It wouldn’t mean ‘everyone would be treated the same’, more that staff would be trained to understand the plethora of issues that can create a stigmatising environment.
This seems to be a really intriguing way to tackle such a huge issue. It doesn’t just relate to STIs and BBVs, but anything: obesity, gender, race, religion, etc. It is certainly a huge task ahead of the project team, but one that needs to happen.


The last day started with a hugely thought-provoking talk by Dr David Carter from the University of NSW, who is leading the Health+Law Research Partnership, which aims to improve access to justice and high quality of life for those living with hepatitis B or HIV in Australia by removing legal barriers to testing and treatment. He was able to connect everyday goings-on to the laws that surround us on a daily basis; laws which we probably don’t even think about, but that, for people living with hepatitis B or HIV, are regularly confronting, and often with negative impacts. The Health+Law team have conducted interviews with people living with hepatitis B to ascertain the legal issues they have had in the past, and what would better support them into the future.
Following David’s presentation, Dr Jacqui Richmond and Dr Amanda Wade presented on GP perspectives on hepatitis B models of care in a low-prevalence area in regional Victoria. They have conducted semi-structured interviews with key hepatitis B healthcare providers in the Barwon South West region, and found that hepatitis B was perceived to be a rare, complex condition by the GPs, which affected their confidence to independently manage patients.
Of the 20 interviewees, six were trained hepatitis B s100 prescribers, but none of them had prescribed treatment and were not confident to do so without consulting a specialist. They reported that GPs in low-prevalence areas or those with low caseloads need support, and one of those supports included collaboration with a specialist nurse to build their confidence and access to case management and clinic audit support.
Dr Jacqui Richmond also presented at the final tabletop session and discussed how there was a huge underrepresentation of nurses and the work that nurses do. One of the reasons for this was that the majority of the work that nurses completed—the follow-up phone calls, the home visits, the talking with families—is not recorded, so their work was underreported and thus undervalued. Jacqui stated that this needs to be done better so data collection occurs and the highly valuable work that nurses are doing is captured, and there is evidence to support expanding the workforce. Jacqui also stated that nurses have done a lot to get to where we are today with our elimination efforts, but this is still not being recognised.
All in all, it was such a wonderful conference, and I am fortunate to have been able to go. The next Viral Hepatitis Conference is to be held in August 2025 on Narrm Country in Melbourne, we hope to see you all there.
Last updated 12 September 2024
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates