The blood–brain barrier is a hugely effective “wall” that protects the brain from pathogens in a person’s body. It’s like a highly selective, very fine sieve that allows vital nutrients and other chemicals that the brain needs to be taken from the blood supply, while keeping out a vast number of dangerous molecules and diseases.
Past research has suggested that psychiatric illnesses such as major depression, bipolar disorder or schizophrenia may be sometimes caused or exacerbated by viral infections, but scientists have not been able to find any direct traces of these viruses in the human brain. Some experts have suggested that perhaps this is because the viruses may not attack the brain directly, but may instead target the brain’s lining, or meninges.
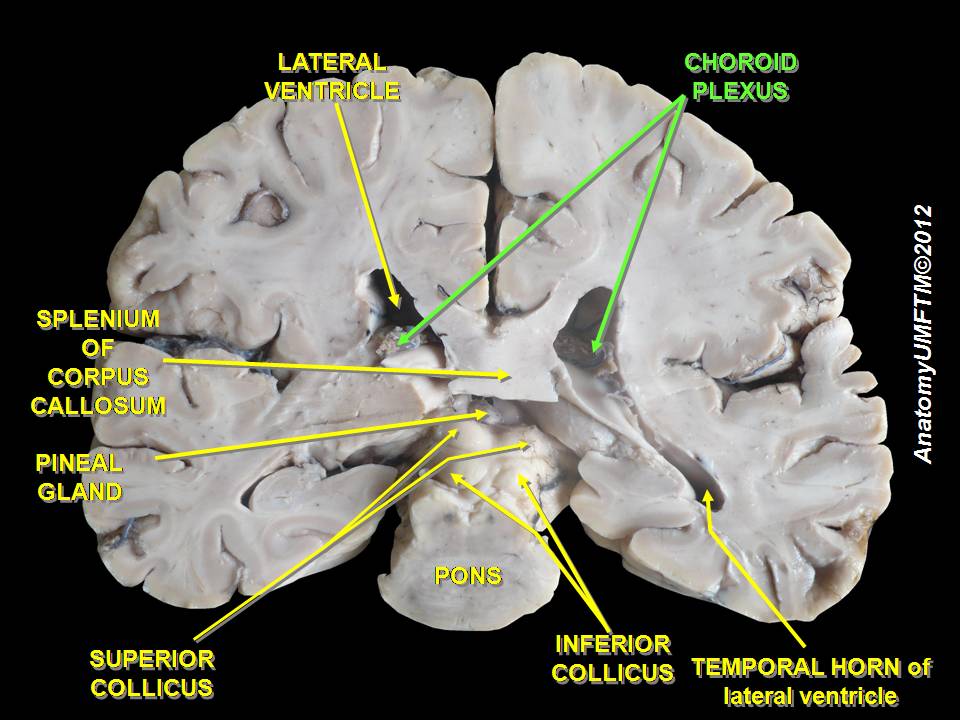
A team of medical scientists at the Johns Hopkins Children’s Center have recently published a study, in the Nature journal Transl3ational Psychiatry, showing that they have evidence of hepatitis C in the human brain’s choroid plexus, a collection of cells that make up the lining of the fluid-filled cavities, or ventricles, which produce the cerebrospinal fluid that protects the brain and spinal cord.
This fits with previous studies which have found that there are much higher than expected rates of hepatitis C infection in people living with schizophrenia or bipolar disorder. The John Hopkins research team, led by neuroscientist Dr Sarven Sabunciyan, suggests that it may be the HCV infections which are associated with the cause of the psychological illnesses, rather than more commonly blamed factors like injecting drug use.
Between 150,000 and 200,000 Australians are living with schizophrenia, while approximately 2.2% of Australians live with a form of bipolar disorder (1 in 50 adult Australians experience bipolar disorder each year).
For the study, the team first analysed choroid plexus samples from postmortem brains of individuals with schizophrenia, bipolar disorder or major depression, as well as unaffected controls. The samples were obtained from the Stanley Medical Research Institute collection, a repository of brain tissue donated after death from people with mental health disorders.

Since past research had failed to find viruses inside the brain tissue itself, the researchers specifically focused on the choroid plexus, and their analysis revealed the presence of various viruses there. The researchers found that more viruses were present in samples from people with schizophrenia or bipolar disorder. But, unlike other viruses, HCV was only present in the brain lining of people who had schizophrenia or bipolar disorder. Notably, the virus was not present in some individuals who were known to have been living with chronic HCV, suggesting that the infection does not automatically spread to the brain lining in every infected person.
During the next phase of the study, the research team analysed a large sample of electronic health records, and found that HCV was documented in 3.6% of those with schizophrenia and 3.9% of those with bipolar disorder — almost double that of those with major depression (1.8%), and approximately seven times that in the control population (0.5%). The researchers say while illicit drug use is common among people with all three disorders, drug use did not account for the higher prevalence of HCV in schizophrenia and bipolar disorder compared with major depression.
The team also looked for viral RNA in sequencing data from the hippocampus, a region of the brain that supports learning, memory and other functions, of subjects identified to have HCV, and found that the virus was absent in this tissue despite being present in the brain lining. However, the presence of HCV in the brain lining altered gene expression in the hippocampus, providing a possible mechanism by which an infection in the lining can affect brain functions and behavior without the virus itself penetrating into the brain.
Our findings show that it’s possible that some people may be having psychiatric symptoms because they have an [hepatitis C] infection
While the researchers caution that their study does not mean that everyone with schizophrenia or bipolar disorder has an HCV infection, they believe their findings provide compelling support for the existence of the virus in the choroid plexus, and that the implications that come from this are serious.
“Our findings show that it’s possible that some people may be having psychiatric symptoms because they have an infection,” Dr Sarven Sabunciyan explained, “and since the hepatitis C infection is treatable, it might be possible for these patients to be treated with antiviral drugs and not have to deal with psychiatric symptoms.”
Dr Sabunciyan now wants to work with mental health professionals to screen for HCV in people with bipolar disorder and schizophrenia. If treating hepatitis C in these patients also eases or cures their psychiatric issues, this would be an amazing extra ‘side-effect’ of the extremely effective hep C cures currently available, and a powerful new reason for everyone to get tested and treated today!
Last updated 20 October 2025
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates