A widely-acclaimed community-led Northern Territory health program which closed the gap for hepatitis B is calling for ongoing support for screening, treatment pathways and workforce capacity building, so that hard-earned improvements will not be lost.
The organisations behind the program, Menzies School of Health Research (Menzies) and Aboriginal Medical Services Alliance Norther Territory (AMSANT), say sustained funding is essential as liver cancer rates continue to rise.
Lead researcher, Professor Jane Davies, said, “We are on the right trajectory, but without ongoing support for screening, treatment pathways and workforce capacity, we risk losing the gains we’ve worked so hard to achieve.” (See update on funding)
Hep B PAST*, launched in 2018 after years of groundwork with remote communities, concluded in 2023 with impressive results validating its culturally safe, community-centred, and led, model of care.
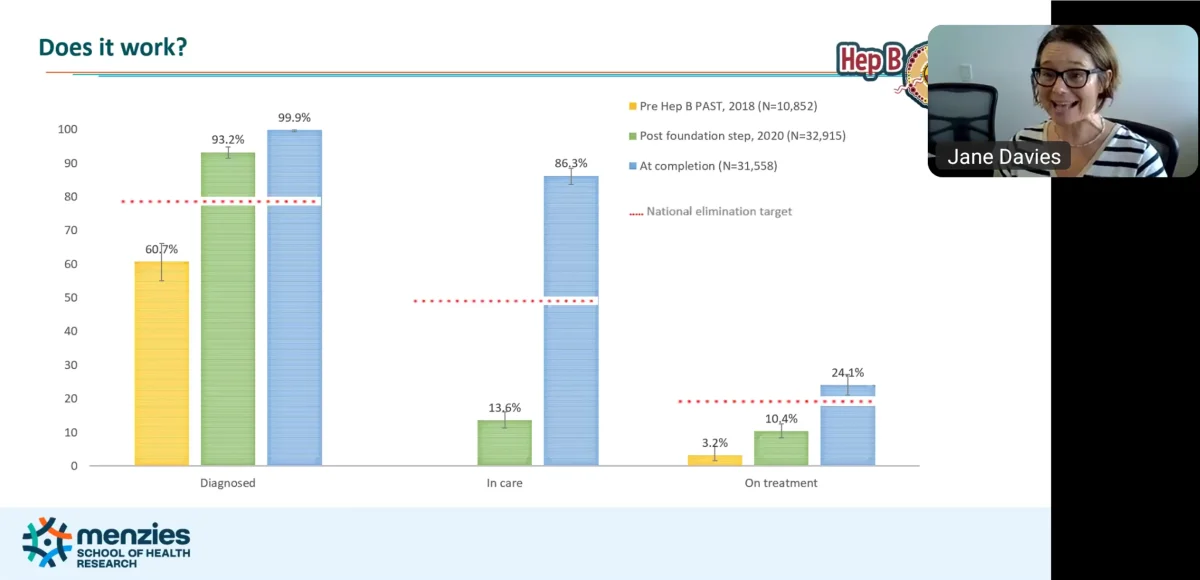
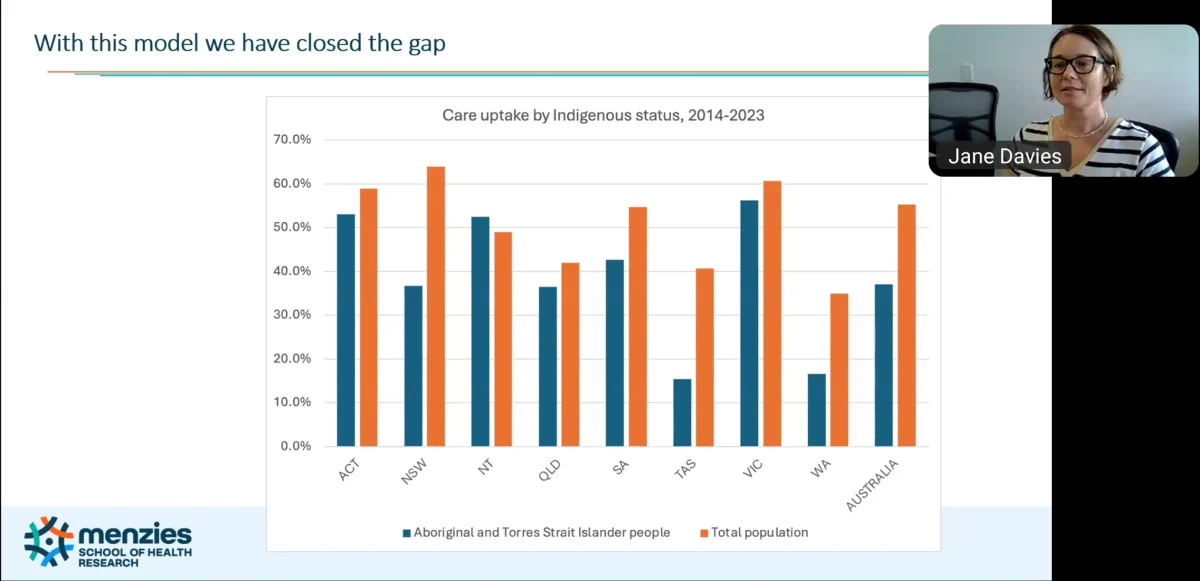
Presenting at the WHO-WHA West Pacific Regional Forum last week, Prof. Davies said with over 50 per cent of Indigenous people with chronic hepatitis B (CHB) in care, the Northern Territory (NT) has “closed the gap”… and, with the rate in the general community at less than 50 per cent, the project had even managed to “flip” the numbers.
New data shows the NT has recorded the largest decrease in hepatitis B mortality of any Australian jurisdiction and that improvement aligns with the expansion of the Hep B PAST program and its companion workforce training, Managing Hepatitis B.
The NT has also exceeded the national hepatitis B elimination targets for diagnosis, care and treatment with 99.9 per cent diagnosed, 86.3 per cent in care and 24.1 per cent receiving treatment. The national targets in the National Hepatitis B Strategy were: 80 per cent diagnosed, 50 per cent in care and 20 per cent receiving treatment.
Both Hep B PAST and Managing Hepatitis B are now recognised nationally as leading models for early detection and culturally safe chronic hepatitis B care.
Prof. Davies said Aboriginal and Torres Strait Islander people in the NT are six times more likely to get liver cancer and chronic hepatitis B is the primary cause.
The prevalence of chronic hepatitis B among Aboriginal and Torres Strait Islander people in the NT is estimated at 6.1 per cent, compared to 1.79 per cent in the territory’s general population.
“Although Australia has among the highest cancer survival rates globally, significant disparity in outcomes persist among Aboriginal and Torres Strait Islander people,” she said.
“Aboriginal and Torres Strait Islander are often diagnosed with more advanced cancer, receive less treatment and have 30 per cent higher mortality rate.”
PAST adopted a two-pronged approach: One was to improve health literacy about hepatitis B amongst Aboriginal and Torres Strait Islander communities with an easy to understand, culturally appropriate digital interactive tool available in 11 languages that cover 70 per cent of the NT indigenous population.
The other was to transition chronic hepatitis B care into the primary care settings using the chronic disease model.
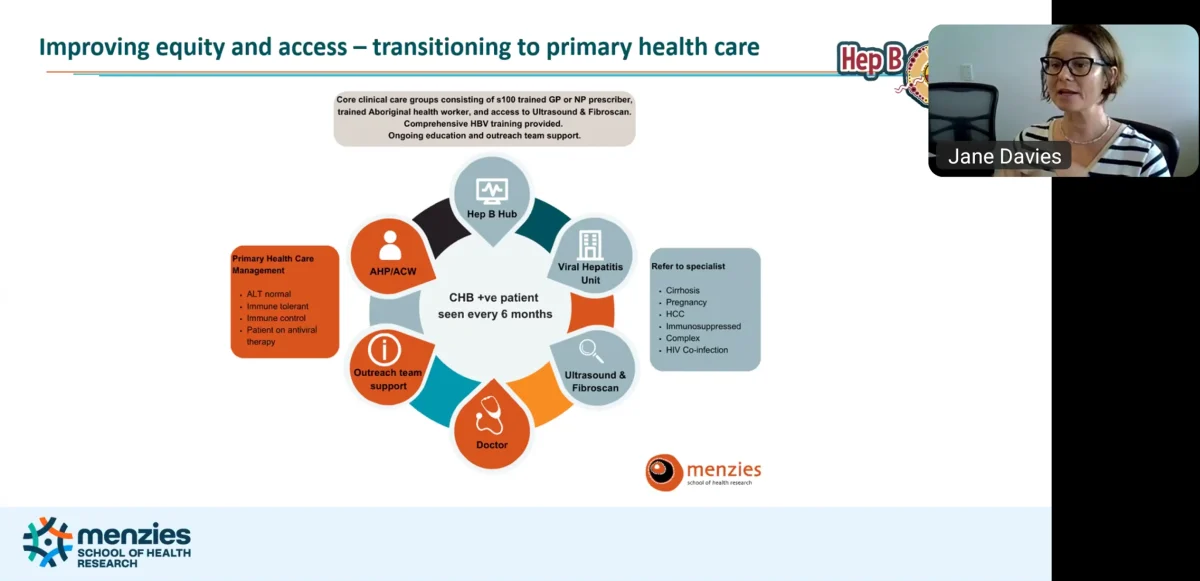
“So chronic hepatitis B now sits alongside diabetes, heart disease, asthma, osteoporosis, and arthritis. This normalises the condition, and reduces stigma… and it becomes part of the usual diseases that primary care workers are trained to identify and provide care for,” said Professor Davies.
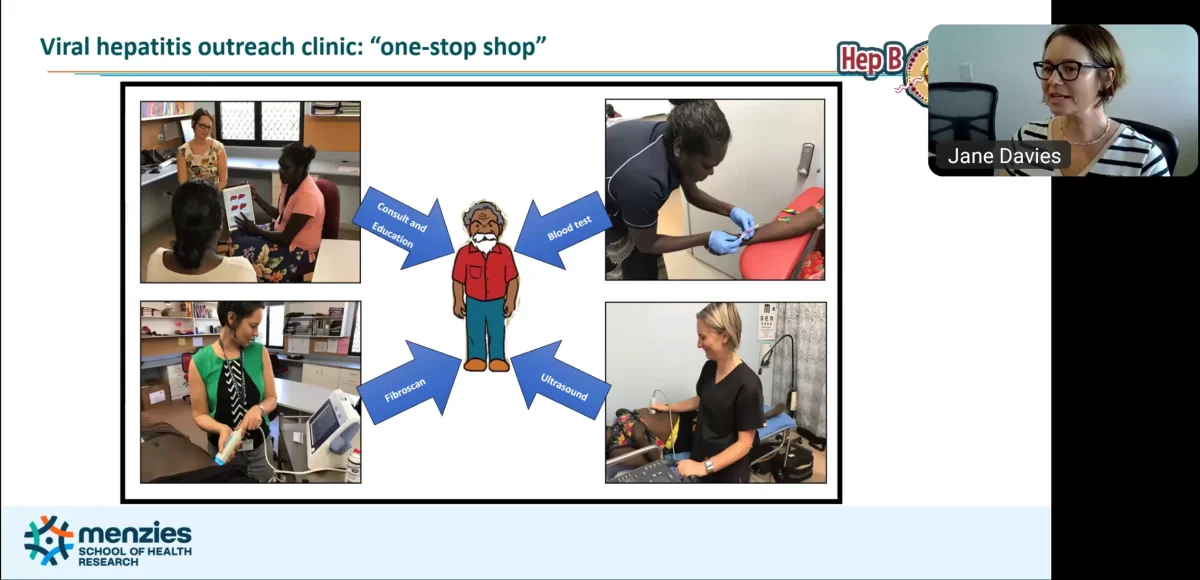
Chronic hepatitis B care is offered directly in remote communities in a “one-stop liver shop” that provides providing blood tests, ultrasounds and follow-up care in a single visit, delivered in partnership with Aboriginal community-controlled health services (ACCHSs).
Those with chronic hepatitis B are seen every six months with care provided by a trained s100 prescriber GP or Nurse Practitioner Prescriber and trained Aboriginal health worker, with access to ultrasound, fibroscan and specialist support for more complex cases such as cirrhosis, pregnancy, liver cancer or co-infections.
The primary care teams receive comprehensive hepatitis B training and ongoing education and support.
Results from the Hep B PAST program has been stunning to say the least.
Deputy lead, Dr Paula Binks, said, “People are being diagnosed earlier, receiving appropriate treatment, and staying engaged in care—and that simply wasn’t happening before.”
“The data shows liver cancer survival for Aboriginal people in the NT has tripled since 2006,” Professor Davies said. “This is an extraordinary shift, and it reflects the combined impact of early detection, patient-centred care and the trust and knowledge built through Hep B PAST and targeted workforce training.”
According to Menzies and AMSANT, the companion Managing Hepatitis B training program—co-designed with Aboriginal health workers—has trained more than 200 workers across the NT.

Prof. Davies said Hep B PAST succeeded because of the persistence, passion, positivity and partnership.
The program strengthens local workforce capability and health literacy, ensuring Aboriginal health workers remain central to diagnosis, education and long-term care. Managing Hepatitis B is now accredited and has expanded to Far North Queensland, with requests from Western Australia.
AMSANT Chair, Rob McPhee, said the results show what is possible when Aboriginal-led, community-controlled models are properly resourced.
“This is an NT success story. We know that Aboriginal people are too often diagnosed later, receive less treatment and experience higher mortality.
“Hep B PAST shows that when we invest in local leadership, language, trust and community-designed programs, we can turn that story around.
“This is exactly what Closing the Gap looks like in practice.”
UPDATE: The Government has committed $1.8 million over three years to Hep B PAST in the 2025 Closing the Gap report.
*Acronym for ‘Hep B – Partnership Approach to Sustainably eliminating Chronic Hepatitis B in the Northern Territory (NT)‘
Last updated 26 February 2026
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates