The incidence of primary liver cancer in Australia has quadrupled since 1982—faster than any other cancer. Yet, the 5-year survival remains just 22%, in stark contrast to countries like Japan, where coordinated surveillance and early detection efforts have dramatically improved outcomes.
A new peer-reviewed article in the Medical Journal of Australia (co-authored by some of Australia’s leading liver health experts) outlines five urgent actions needed to change this trajectory:
- Support a nationwide campaign for liver disease health promotion, in partnership with community organisations
- Establish and fund a national approach to chronic liver disease screening and linkage to care, including timely access to liver fibrosis assessment
- Establish and fund a national HCC risk registry and surveillance program
- Fast-track approval and integration of blood-based biomarkers into HCC surveillance programs
- Set clear national targets for liver disease screening and assessment, HCC surveillance uptake, and HCC mortality.
Hepatocellular carcinoma (HCC) accounts for over 85% of primary liver cancers, and usually develops in the setting of chronic liver disease, with up to 90% of cases occurring in people with liver cirrhosis. It is usually caused by viral hepatitis, alcohol‐related liver disease or metabolic dysfunction‐associated fatty liver disease (MAFLD). Importantly, when detected early, the cure rate for HCC is very high. In Australia, at-risk individuals should get 6-monthly liver ultrasounds, but this often does not happen.
Due to a low uptake of surveillance, most HCC cases are only detected at an advanced stage when only palliative treatments can be offered. Data from Melbourne show minimal change in the proportion of new HCC cases diagnosed through surveillance over the past decade, from 40% in 2013 to 39% in 2022. This is primarily due to lack of awareness among health workers and the community about who is actually at risk of chronic liver disease or HCC, the often asymptomatic nature of the early stages of chronic liver disease and HCC, a lack of awareness of the survival benefits of HCC surveillance for individuals at risk, and lack of access to HCC surveillance.
As you might sadly expect, the impact of late diagnosis of HCC on mortality is even more striking among people who face barriers to care, including First Nations Australians and those who experience social and health disadvantages.
But compare these alarming facts with those in some east Asian nations, where in the first two decades of this century both the incidence and mortality of primary liver cancer have fallen, reflecting successful preventive health initiatives that address viral hepatitis, such as hepatitis B vaccination and treatment, and hepatitis C cure. Importantly, however, it also reflects better early diagnosis and increased use of curative treatment.
In Australia, we have national surveillance programs for bowel, cervical and breast cancer, but we have no national population‐level screening programs for chronic liver disease and no national HCC surveillance program.
The study focused on Japan as an example. In Japan, access to HCC surveillance and improvements in diagnostic methods and treatments have seen a dramatic improvement in 5‐year survival from 5% in 1980 up to 43% in 2005 and 58% in 2013.
In Australia, implementation of advances in public health interventions for chronic liver disease, surveillance, diagnostic methods and treatments has followed a similar trajectory to Japan, but HCC survival has remained stubbornly low (currently sitting at 22%). What can Australia learn from countries such as Japan, who have seen such impressive reductions in HCC mortality?
Since the 1980s, Japan has had a national HCC surveillance program, with annual education of GPs and health promotion campaigns for the general population about HCC and its risk factors being supported and financed by the Japanese Ministry of Health since 1999. Importantly, this program was embedded within pre‐existing national screening and treatment programs for viral hepatitis, facilitating early assessment for liver cirrhosis and linkage into HCC surveillance. In Australia, we have national surveillance programs for bowel, cervical and breast cancer, but we have no national population‐level screening programs for chronic liver disease and no national HCC surveillance program.

Japan’s HCC program also includes delivery of surveillance via a national HCC risk registry and community‐based HCC surveillance centres and hospital settings at a minimal cost. Although as a geographically small and concentrated nation Japan has fewer geographical challenges to negotiate in delivery of its HCC program compared with Australia, centralised organisation of HCC surveillance with decentralised imaging delivery in clinics has proven effective to improve access to high quality HCC surveillance. In Australia, data from Victoria showed that during the early years of the COVID-19 pandemic, there was a shift from hospital-based to community‐based radiology services to deliver hepatology clinic‐led HCC surveillance programs. This resulted in no significant reduction in HCC detection rates, suggesting a similar model could work well nationwide.
In Japan, those with viral hepatitis‐related cirrhosis are considered very high risk for HCC and have short‐interval surveillance every three to four months, combined with a dynamic computed tomography (CT) or magnetic resonance imaging (MRI) scan supported at a doctor’s discretion, which is significantly more frequent and thorough than the six-monthly ultrasounds recommended in Australia.
Based on what has proven effective in Japan, the study makes the five recommendations listed above.
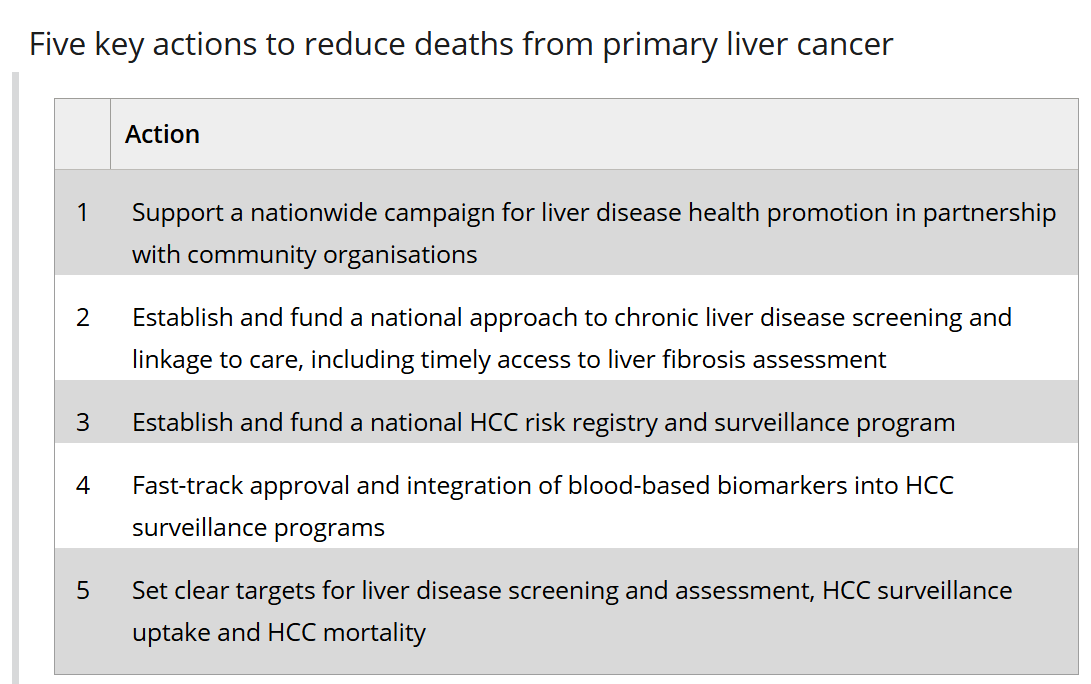
Despite Australia having ready access to advanced treatments for HCC in Australia, many lives are lost due to late detection. Increasing assessment for liver disease and cirrhosis in primary care, coupled with a strong, funded national HCC surveillance program using ultrasound and blood biomarkers, is vital if we want to reduce deaths from HCC.
Last updated 18 August 2025
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates