Aboriginal and Torres Strait Islander people experience a greater burden of disease related to blood-borne viruses (BBV) and sexually transmitted infections (STI). In recognition of this alarming reality, Australia has in place an official National Aboriginal and Torres Strait Islander BBV and STI Strategy, backed by the federal government and endorsed by the health ministers of all Australian states and territories.
This strategy is updated every five years, and the most recent completed version, the Fifth, which covered the years 2018–2022, is being investigated in order to find out just how well it’s working.
The goals of the Fifth National Aboriginal and Torres Strait Islander BBV and STI Strategy are to:
- Reduce the transmission of blood-borne viruses (BBV) and sexually transmissible infections (STI) among Aboriginal and Torres Strait Islander people;
- Close the gap in BBV and STI incidence, prevalence, testing and treatment rates between Aboriginal and Torres Strait Islander and non-Indigenous populations;
- Reduce morbidity and mortality related to BBV and STI;
- Minimise the personal and social impact of BBV and STI;
- Minimise the negative impact of stigma, racism, discrimination, and legal and human rights issues on Aboriginal and Torres Strait Islander people’s health.
…there are serious gaps in how to even measure some of the needed data to see things are improving,
The National Aboriginal and Torres Strait Islander BBV and STI Strategy has 14 targets that provide specific focus for the efforts made towards achieving the goals of this Strategy. Each target has corresponding indicators that measure progress towards attaining the target. Not all the goals are related to viral hepatitis, but to other infections like HIV, congenital syphilis or gonorrhoea. For information on those measures not discussed here, go here.
For the specific measures concerning viral hepatitis, the news is mostly good, but it could also be a lot better. Furthermore, there are serious gaps in how to even measure some of the needed data to see things are improving, to the point that a few parts of the plan risk remaining “motherhood” statements–things everyone agrees are good, but nobody actually has a concrete way to make sure they actually happen.

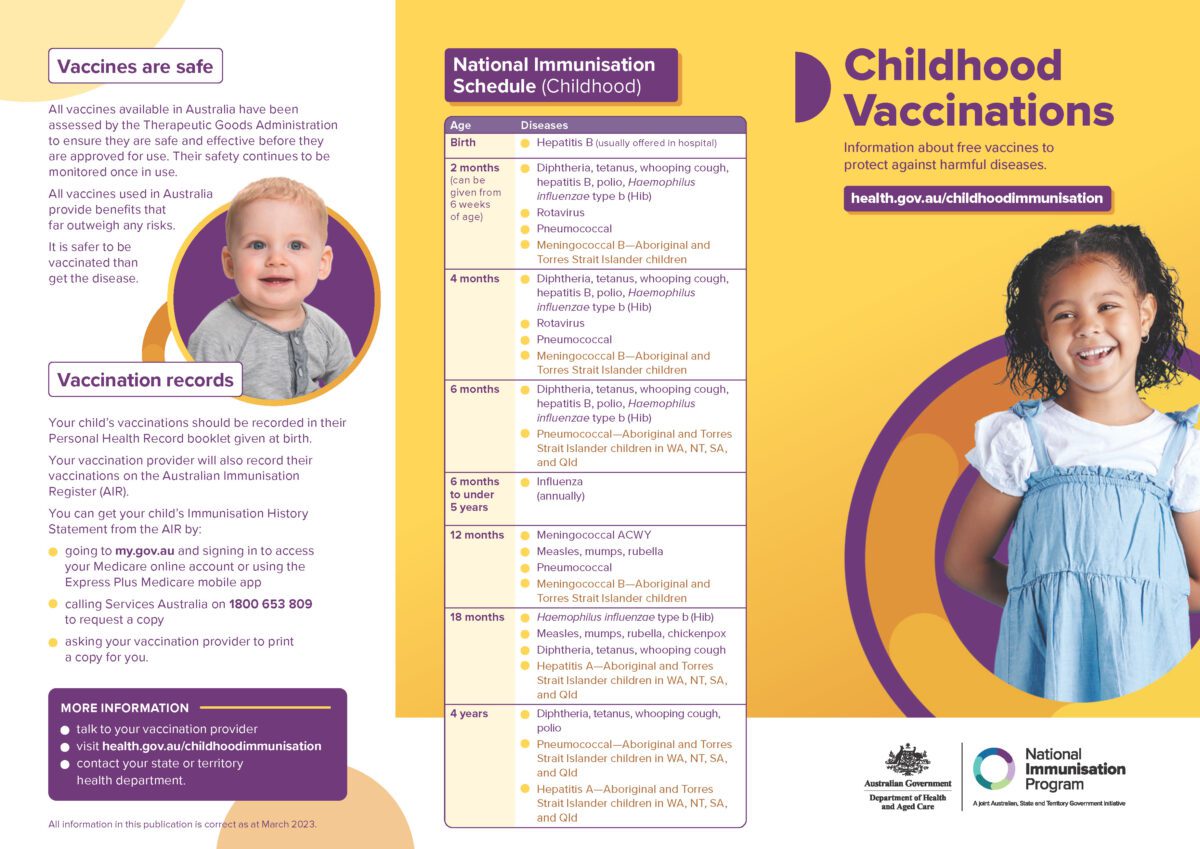
PLAN: Achieve and maintain hepatitis B childhood vaccination coverage of 95% at 12 and 24 months of age
Between 2017 and 2022, among Aboriginal and Torres Strait Islander children aged 12 months, the target of 95% hepatitis B vaccination coverage was reached in 2017 not in subsequent years, 2018–2022, with a coverage rate of 90% reported in 2020. Among Aboriginal and Torres Strait Islander children aged 24 months, hepatitis B vaccination coverage of 95% was reached for all years 2017 to 2022 with a coverage rate of 96% reported in 2022.
PLAN: Reduce the number of newly acquired hepatitis C infections by 60%
The Australian Needle and Syringe Program Survey (ANSPS) provides serial point prevalence estimates of HIV and hepatitis C antibody prevalence, hepatitis C RNA prevalence, and monitors sexual and injecting behaviour among people who inject drugs in Australia. Among Aboriginal and Torres Strait Islander participants in the ANSPS, the proportion of people with evidence of past or current hepatitis C infection declined from 69.9% in 2015 to 35.7% in 2022. By comparison, the proportion of participants with evidence of current hepatitis C infection declined from 50.7% in 2015 to 12.2% in 2022.
PLAN: Increase the proportion of people living with hepatitis C who are diagnosed to 90% and the cumulative proportion who have initiated direct acting antiviral treatment to 65%
Data relating to the estimated proportion of Indigenous people with chronic hepatitis C who have been diagnosed were not available over the lifetime of the strategy. Estimates of the numbers of people living with hepatitis C can be generated using numbers of people newly diagnosed (given here as notification rates), numbers of tests resulting in a positive result, and the numbers of people receiving treatment. These estimates are in development and were unavailable throughout the reporting period. In lieu these data, data relating to other indicators for the same target are presented below.
- Notification rates: Between 2018 and 2022 the hepatitis C notification rate among Aboriginal and Torres Strait Islander people fluctuated, including a decline in notifications in 2020, likely related to the COVID-19 pandemic. In 2022 the hepatitis C notification rate was 156.2 per 100 000. This trend was similar among Aboriginal and Torres Strait Islander males and females and in 2022, the hepatitis C notification rate was 216.2 and 95.5 per 100 000 respectively.
…32% of participants reported ever having a hepatitis C tests in 2020, down 42% from in 2013.
- Testing: Of Aboriginal and Torres Strait Islander ANSPS participants, the proportion reporting a hepatitis C test in the previous 12 months remained stable between 2015 and 2019 and was 59% in 2019 but declined to 51% in 2022. Between 2015 and 2022, the proportion of participants who reported ever having had a hepatitis C test fluctuated between 76% and 86% and was 78% in 2022.
- Among young people participating in the 2020 Goanna Survey, 23% of participants reported having had a hepatitis C test in the previous 12 months, down from 32% in 2013. In the same survey, 32% of participants reported ever having a hepatitis C tests in 2020, down 42% from in 2013.
- Treatment: Of Aboriginal and Torres Strait Islander people participating in the ANSPS, 66% of participants reported ever having had hepatitis C antiviral treatment in 2022, up from 10% in 2015. By comparison, 27% of respondents reported having had antiviral treatment in the previous 12 months in 2022, a considerable increase on the 1% reported in 2015, but down from 39% in 2019. The significant increase in the proportion of participants reporting ever having had antiviral treatment relates to the widespread availability of direct-acting antiviral treatment, subsidised since 2016.
- The data relating to Indicator 8i: Proportion of Indigenous people entering custodial settings who reported having any hepatitis C antiviral treatment and Indicator 8j: Proportion of young (16-29 years) Indigenous people who reported having had hepatitis C antiviral treatment are in development and were unavailable throughout the reporting period.
PLAN: Reduce hepatitis C attributable mortality by 30%
Data required to report on this indicator were not available over the lifetime of the strategy.
PLAN: Increase the proportion of people living with hepatitis B who are diagnosed to 80%, receiving care to 50%, and on antiviral treatment to 20%
While modelled estimates of the total number of Aboriginal and Torres Strait Islander people living with chronic hepatitis B, in care and receiving treatment are not currently available, investigation is underway to source appropriate datasets to inform future estimates. In lieu of these estimates, hepatitis B notification rates for Aboriginal and Torres Strait Islander people are presented in this section. Data relating to Indicator 10b: Proportion of Indigenous people entering custodial settings with evidence of past or present hepatitis B infection also relate to this indicator are in development and were unavailable throughout the reporting period.
- Among Aboriginal and Torres Strait Islander peoples, the hepatitis B notification rate declined from 29.4 per 100 000 in 2018 to 19.0 in 2022. A similar trend was seen among males and females with notification rates 25.1 and 13.4 per 100 000 in 2022, respectively.
PLAN: Reduce hepatitis B attributable mortality by 30%
Methods to produce the data to report on this target are in development and were unavailable throughout the reporting period.
PLAN: Reduce the reported experience of stigma among Aboriginal and Torres Strait Islander people with BBV and STI, and the expression of stigma, in relation to BBV and STI status.
Methods to produce the data to report on this target are in development and were unavailable throughout the reporting period.
As you can see, the general trends are mostly positive where they can be measured, but too much remains either unmeasured or else improving but not yet at a satisfactory level. If we are to eliminate viral hepatitis by 2030, which is Australia’s official goal, we need to redouble our efforts, especially for Indigenous communities.
Last updated 25 October 2024
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates