The recent concern about fatal opioid overdose from nitazenes in the illicit drug supply has raised fears for many prison experts. People who are in prison are not afforded the same protections as people in the community while recent release from prison is also an extremely vulnerable time in which many people experience fatal overdose.
A coalition of health practitioners, harm reduction advocates and experts have called for expanded access to naloxone in prisons to protect against fatal overdoses from nitazenes and other synthetic opioids. In a joint statement, they say in order to prevent avoidable deaths, each state and territory government should immediately:

- Provide training to custodial officers to recognise overdose and administer naloxone
- Ensure naloxone is accessible to custodial officers to promptly and effectively respond to overdose
- Ensure that naloxone and naloxone training is routinely offered to all people exiting prison.
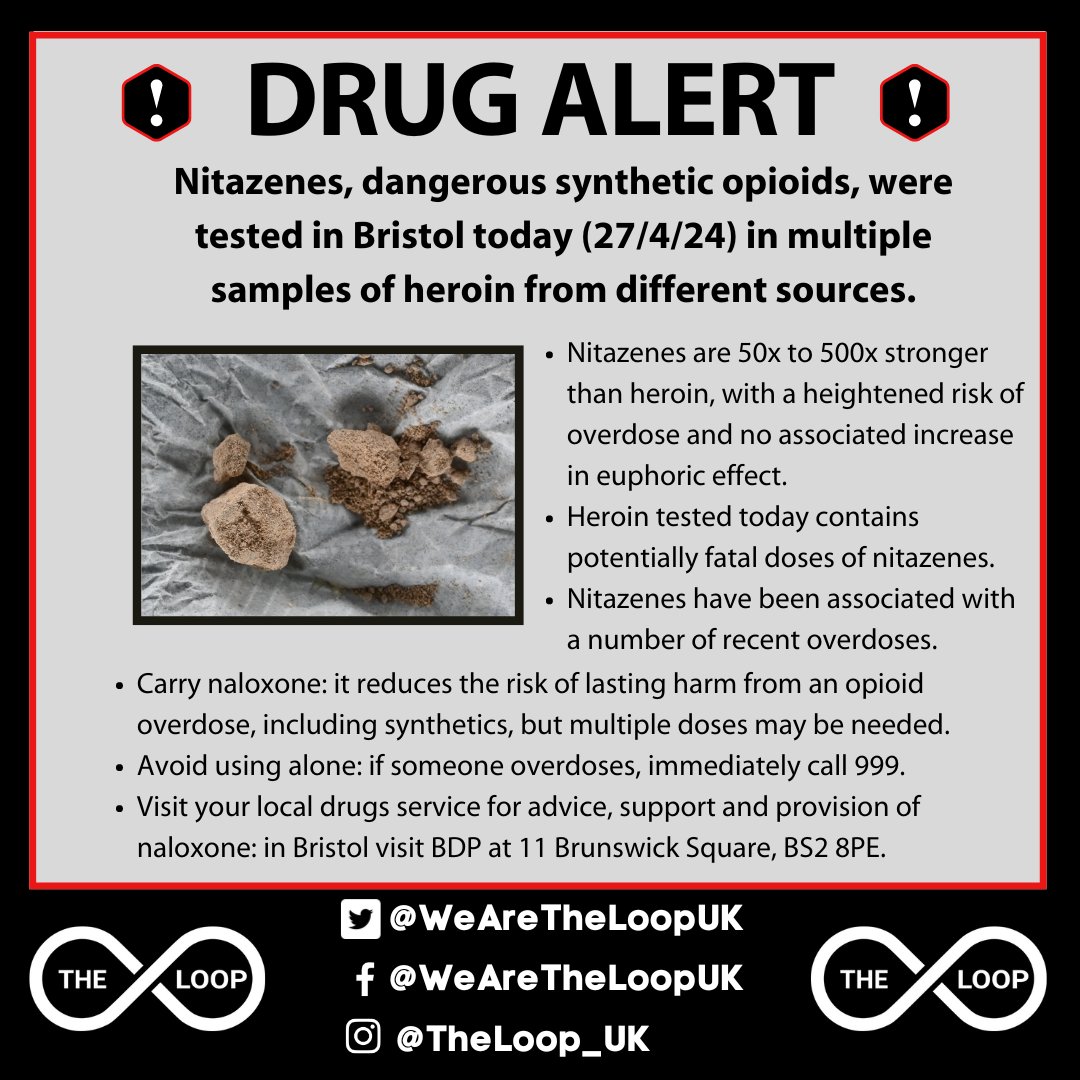
Nitazenes are a synthetic opioid that can be hundreds of times stronger than heroin and can be fatal even in very small amounts. They have been linked to an increasing number of overdoses and deaths in Australia this year and have also been connected to at least 15 overdose deaths in prisons in the UK. With new national data released last week on wastewater analysis, and a NSW Drug Summit now scheduled for later this year, it is a reminder that we should be addressing harms of illicit drug use.
“Nitazenes in prisons are a disaster waiting to happen,” says the CEO of the Australian Alcohol and Other Drugs Council, Ms Melanie Walker. “We know nitazenes are in the illicit drug supply in Australia and it is only a matter of time before they enter prisons.
“People in prison have a higher rate of injecting drug use than the general population and despite efforts to prevent drug supply in prison, the evidence shows that drug use is still common. Nitazenes and other synthetic novel drugs are significantly more difficult to detect than “traditional” opioid drugs such as heroin. Prisons are currently ill equipped to handle a potential influx of these lethal substances,” Ms Walker continued.
A key tool in the fight against opioid overdose is naloxone, a life-saving medication which can temporarily reverse an opioid overdose, including from nitazenes. It is available in Australia as an easy-to-use nasal spray or injection. The Australian Government Department of Health and Aged Care recommends that naloxone be administered to anyone overdosing from opioids.
If we are going to save lives, we must find ways to get naloxone to people in prison when they need it.
However, naloxone is not readily available in prisons in Australia. Naloxone is generally only administered by healthcare staff. As noted by Ms Walker, this severely limits access for people who need it, when they need it: “Health staff are not always available or accessible to people in prison. If we are going to save lives, we must find ways to get naloxone to people in prison when they need it.
“One important step that all prisons could take right now is for custodial officers to have ready access to naloxone and be trained in how to recognise and respond to overdose. Many police officers across Australia now regularly carry and administer naloxone. Custodial officers should be trained in the same way.”
The period following release from prison is an especially high-risk time for overdose, with opioid overdose deaths up to twenty times higher for people leaving prison than the general population. Ensuring that naloxone and training in how to use it is provided to people in prison before release is a key strategy in combatting overdose deaths. However, provision is currently patchy as not every state and territory provides training or access to naloxone for people exiting prison.

“There are too few people getting naloxone at the time they leave prison,” says Ele Morrison, Deputy CEO of the Australian Injecting and Illicit Drug Users League (AIVL).
“To save lives, training and access to naloxone must be expanded and improved within all prisons. As a first step we call on governments to implement these measures immediately. But we also encourage them to look for ways to implement harm reduction in prison.”
The following are signatories to the statement:
- Mary Harrod, CEO, NSW Users and Aids Association (NUAA)
- Geoff Davey, CEO, QuIHN
- Professor Alison Ritter AO, Director, Drug Policy Modelling Program (DPMP), UNSW
- Liz Barrett, Chair, Harm Reduction in Prisons Working Group
- Melanie Walker, CEO, Australian Alcohol and Other Drugs Council (AADC)
- Dr Lise Lafferty, Senior Research Fellow, Centre for Social Research in Health (CSRH), UNSW
- Sione Crawford, CEO, Harm Reduction Victoria
- Professor Kate Dolan, Harm Reduction Australia, UNSW
- John Didlick, Policy Analyst, Hepatitis Australia
- Paul Dessauer, CEO, Peer Based Harm Reduction WA
- Brent Bell, CEO, Hepatitis WA
- Steven Drew, CEO, Hepatitis NSW
- Ele Morrison, Deputy CEO, Australian Injecting and Illicit Drug Users League (AIVL)
Last updated 16 August 2024
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates