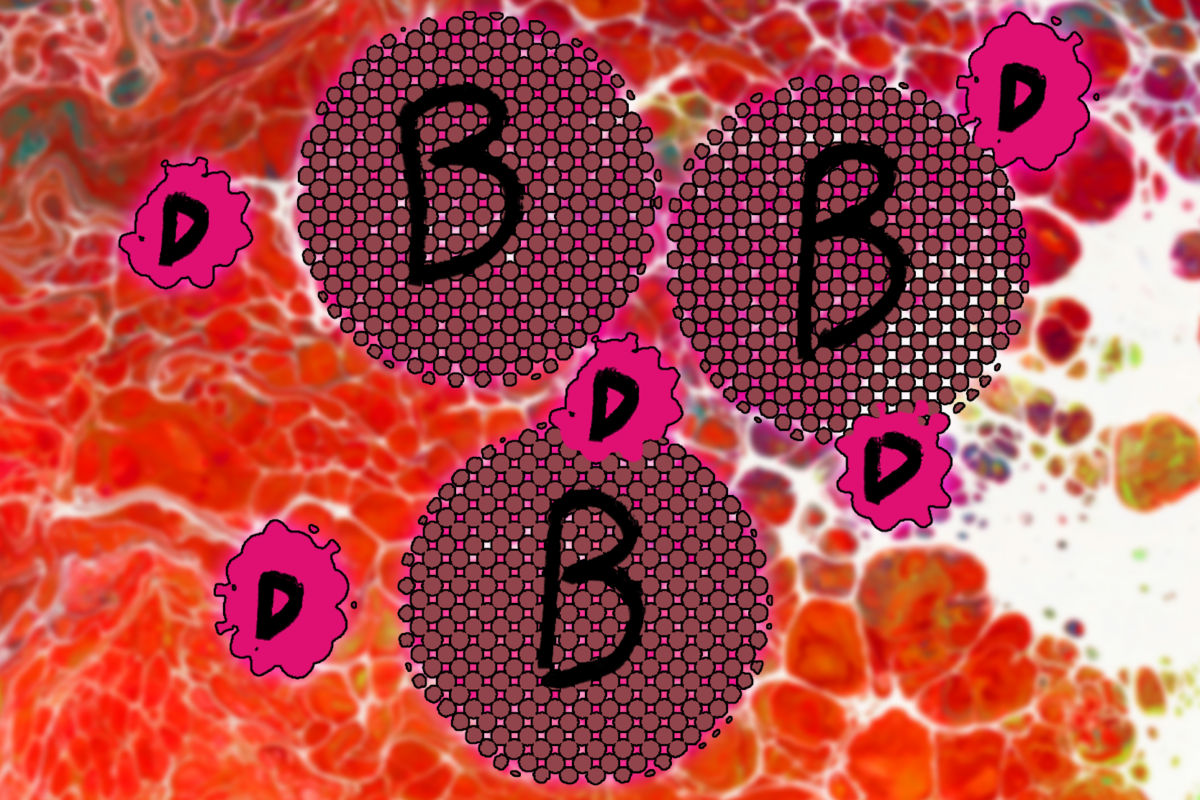
The prevalence rates of mental illness in people living with viral hepatitis are significantly higher than those rates in the general population. Some research suggests that the prevalence of HCV infection in patients with severe mental illness may be as high as nine times that of the general population. This means that someone living with hepatitis B or hepatitis C is much more likely to present at an emergency department with an acute mental illness.
Unfortunately, a serious disconnect between hospital emergency departments and the National Disability Insurance Scheme (NDIS) is failing people with mental health conditions, as new research from the University of South Australia shows that they frequently receive inadequate care within emergency departments, potentially putting thousands of vulnerable people at risk.
Funded by MIND Australia, the study, published in the International Journal of Mental Health Nursing, found that people with psychosocial disabilities (disabilities caused as a result of poor mental health) not only experience distress when dealing with the NDIS, but also face further serious problems when they present to emergency departments requiring emergency care.

Speaking with NDIS participants, the nationwide study found that when participants disclosed that they had NDIS support, clinicians wrongly assumed that the NDIS provides medical and mental health crisis care, which it does not–this is entirely the job of hospital emergency departments.
It’s a concerning finding, particularly following the discrimination, non-inclusivity and lack of equality experienced by people with a disability, identified in the NDIS review and the disability royal commission.
And they don’t see that they’re causing emotional distress… [they say] that there’s this fancy Candyland [NDIS], you can go through and everything will be fixed.
A participant in the study
In Australia, 1.1 million people have a psychosocial disability which causes limitations or restrictions in their everyday activities. Additional, 58 per cent of these people also have a anxiety or emotional condition, 42 per cent have problems with memory or periods of confusion, 41 per cent have behavioural conditions, and 40 per cent have a mental illness (such as schizophrenia). 86 per cent also have at least one other disabling condition (63 per cent physical disability; 38 per cent intellectual disability; and 33 per cent sensory disability).
But the system wasn’t designed for psychosocial disabilities and you can see it…it’s like saying to someone, if you need a critical surgery, do you want to keep your right hand or your leg? Which one?
A participant in the study
UniSA researcher and PhD candidate Heather McIntyre said that the disconnect between the NDIS and emergency departments is failing people with psychosocial disabilities.

“Time and time again we hear about people experiencing distress when they contact the NDIS – they fight to be heard, fight for support, and are often dismissed, so the last thing they need is to go through this again when they require emergency care,” she explained. “This is particularly concerning for people with a mental health condition, especially those with fluctuating psychosocial disabilities who may struggle with communication.
“Because many emergency department staff aren’t aware of the limitations of NDIS supports, they wrongly assume that the NDIS provides a higher level of care than it does. This leaves many people with a psychosocial disability being discharged [from] emergency without appropriate treatment and returned to the situation that caused them to present in the first place.
“It’s an inequitable and unsafe approach that is putting thousands of people at risk.”
The study demonstrates that there is an urgent need to strengthen service integration between the NDIS and emergency departments. “Communication between the two services is not occurring seamlessly, which affects continuity of care. This needs to change,” Heather McIntyre noted.
I find a lot of time you have to fight…It’s a battle…a bit of a full-time job…I keep on top of all the legislation, the wording, the changes…No-one has their facts straight, no-one knows what they’re talking about. There’s not clear information unless you’re researching 24/7 yourself.
A participant in the study
“We must start at the pointy end: emergency department clinicians need more training and education to better understand how the NDIS works and how to best support people with a disability. They need to learn how to support people with neurodiversity and hearing impairments, how to build trust and how to really listen, as well as to provide low sensory environments. But equally, stronger connections and pathways must be established between NDIS providers and emergency departments so that everyone is on the same page.
“With budget cuts to the NDIS of $14 billion over the next four years, peoples’ disability supports will further be reduced, resulting in more emergency department presentations when supports are insufficient. In emergency departments we need to step up care, not ration care, if we are to support people with disabilities who already feel abandoned by the health system.”
Last updated 5 September 2024
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates