The pathway to global elimination of viral hepatitis is “Integration”. This was one of the stand-out messages at the World Hepatitis Summit 2024 (WHS2024) in Lisbon where successful integration strategies were presented. The key to this approach is to make hepatitis screening, monitoring and clinical management part of the broader health system, delivered along with other infectious diseases screening and care.
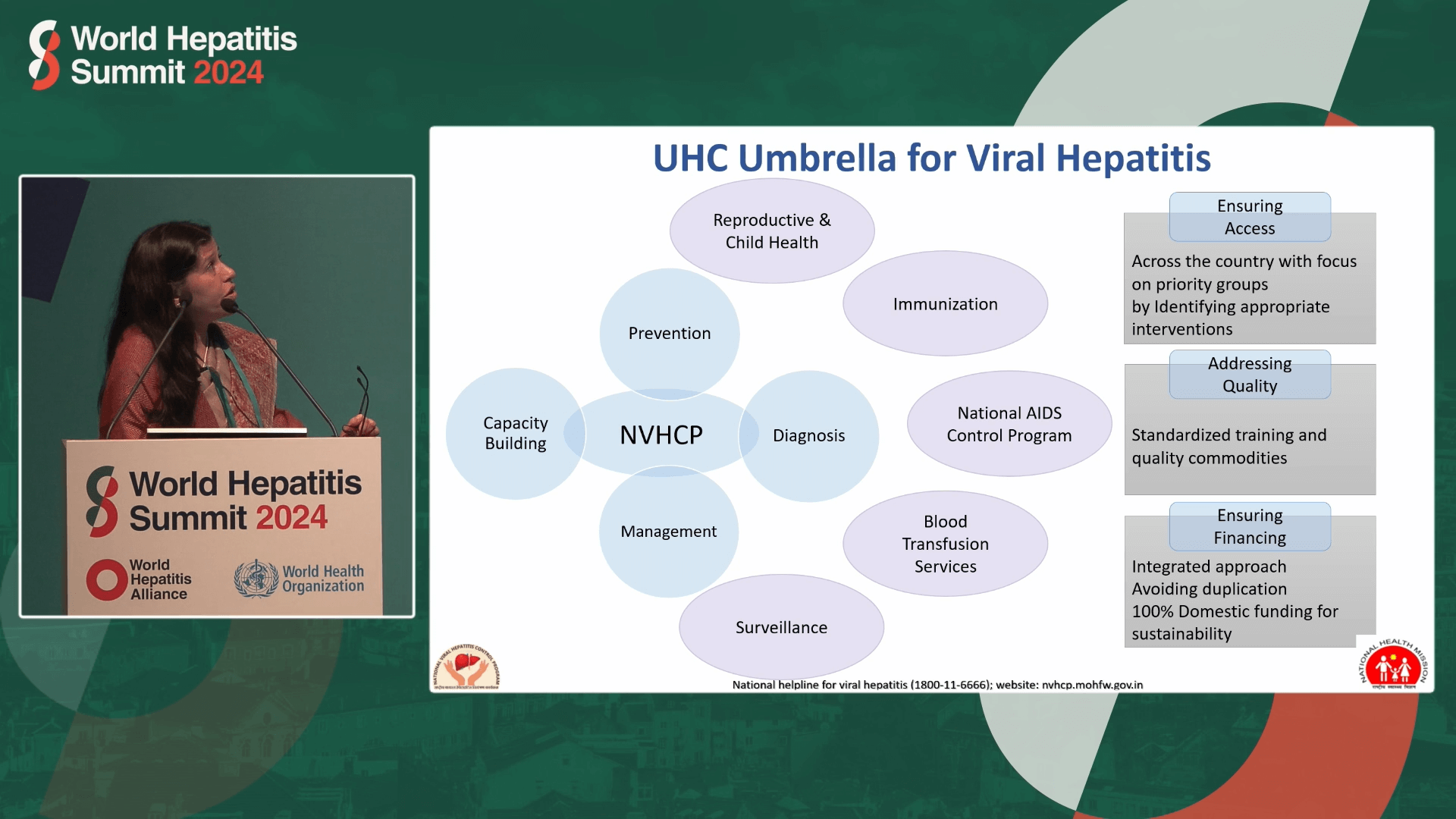
One example is India’s National Viral Hepatitis Control Program (NVHCP) which integrates viral hepatitis prevention, diagnosis and management into existing health services, mobilising the whole health system as a response to reach elimination.
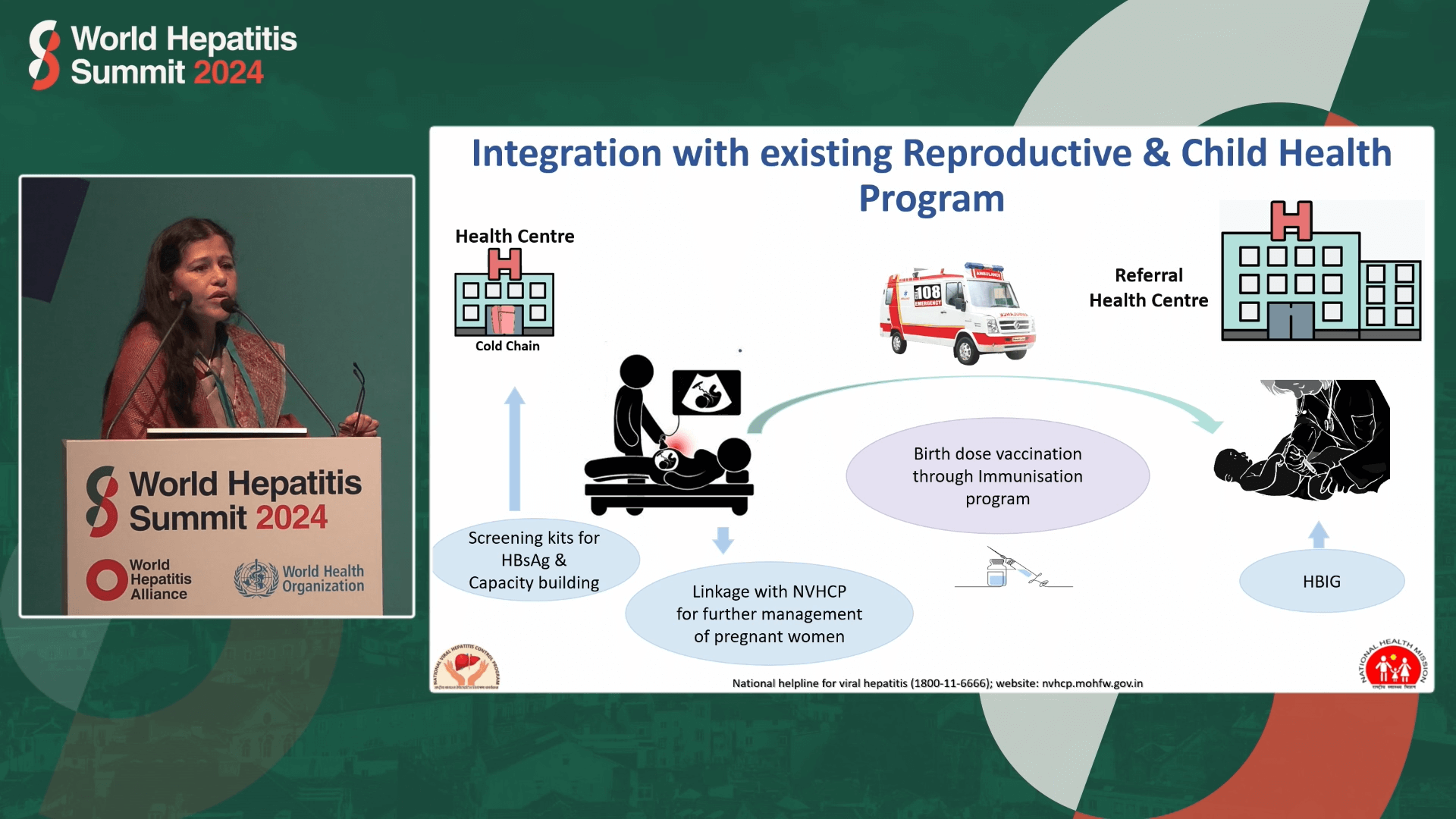
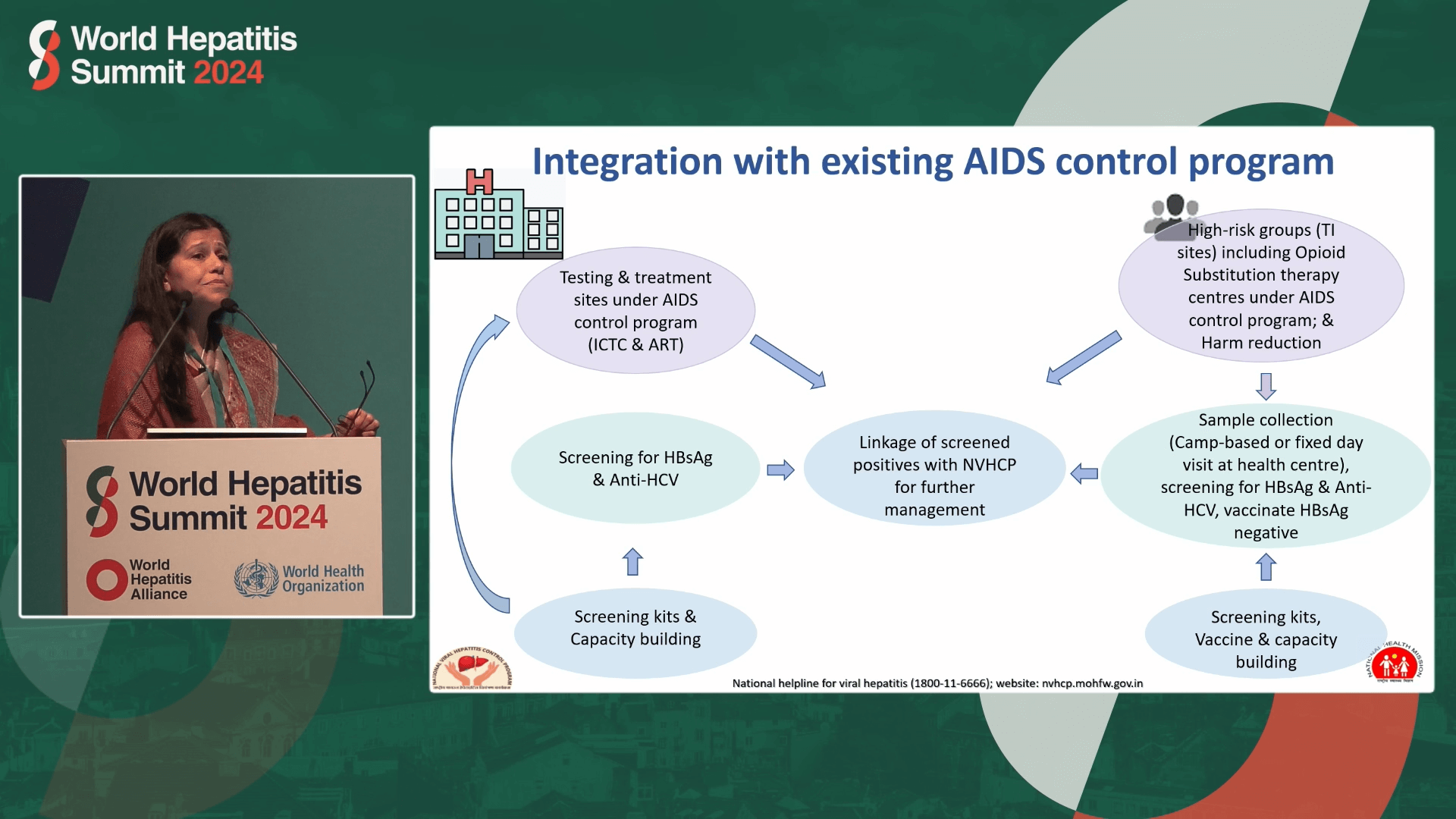
Speaking at the WHS2024 Integrate session on 10 April, Dr. Sandhya Kabra, Deputy Commissioner of the Indian health ministry’s Division of Viral Hepatitis, described the NVHCP strategy as “piggy-backing” on other existing services, such as reproductive and child health immunisation, AIDS control and blood transfusion services.
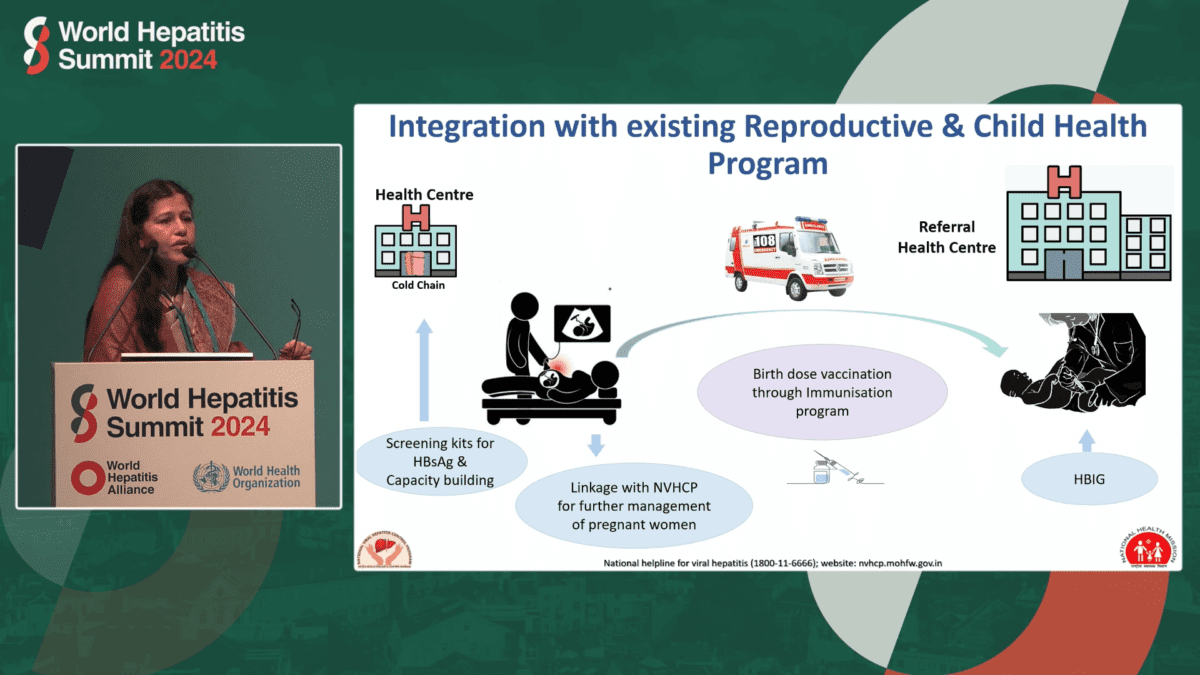
“We use the same infrastructure and staff,” she said, expanding the “capacity” by training existing staff. She said one of the key services the program integrated into was maternity care which has 50,000 community level sites, giving the program access to a crucial target group for hepatitis B vaccination and immunisation.
… we piggybacked on it and made it a hepatitis helpline as well.
The Program also integrated with the Tuberculosis system which had an existing helpline. “So we piggybacked on it and made it a hepatitis helpline as well,” she said.
According to Dr Kabra, when health authorities launched the program, they were “very well aware” they had a “very tough task” ahead to reach elimination by 2030 because the program only started in 2018 and expanded to include hepatitis B in 2019.

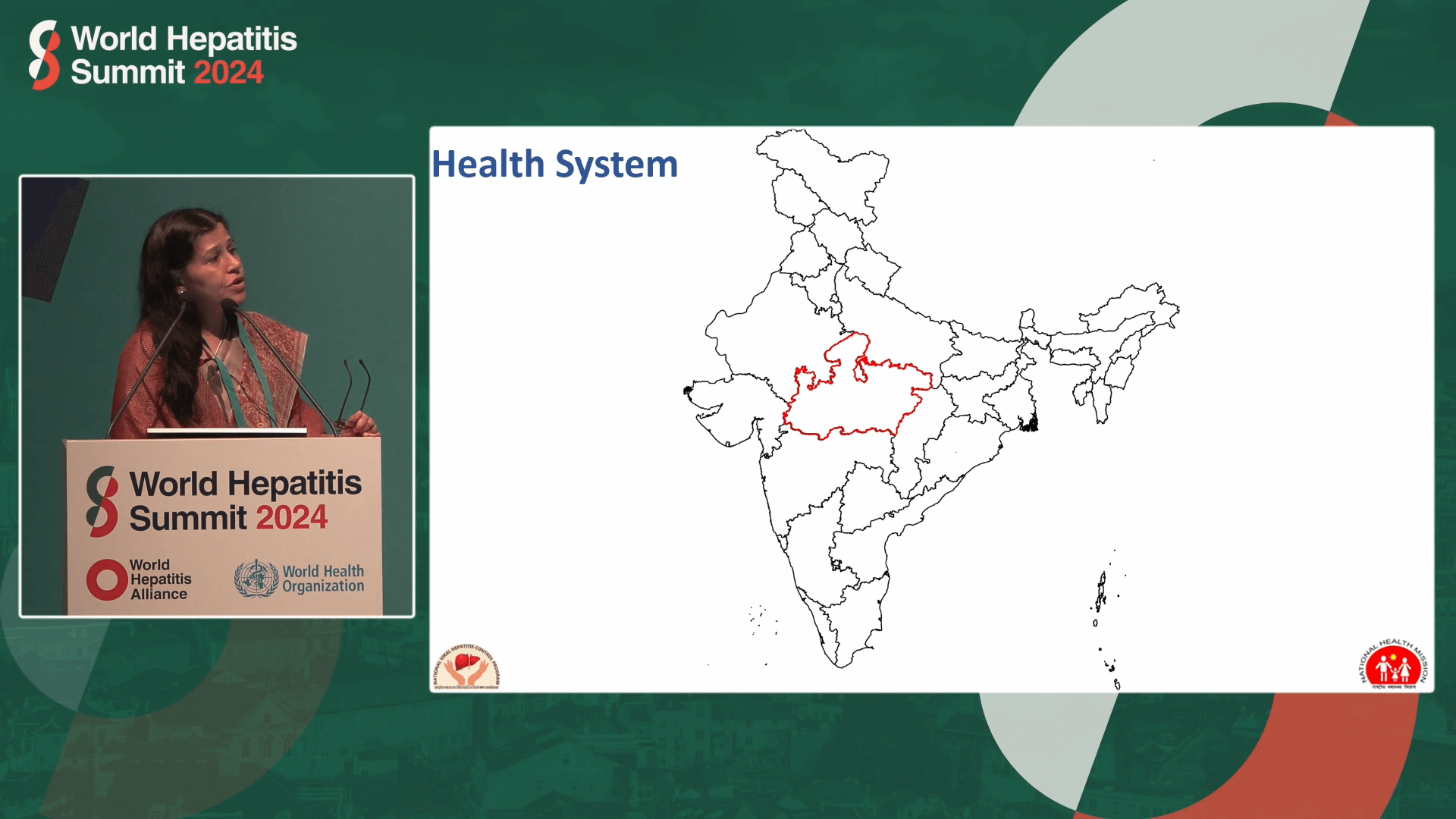
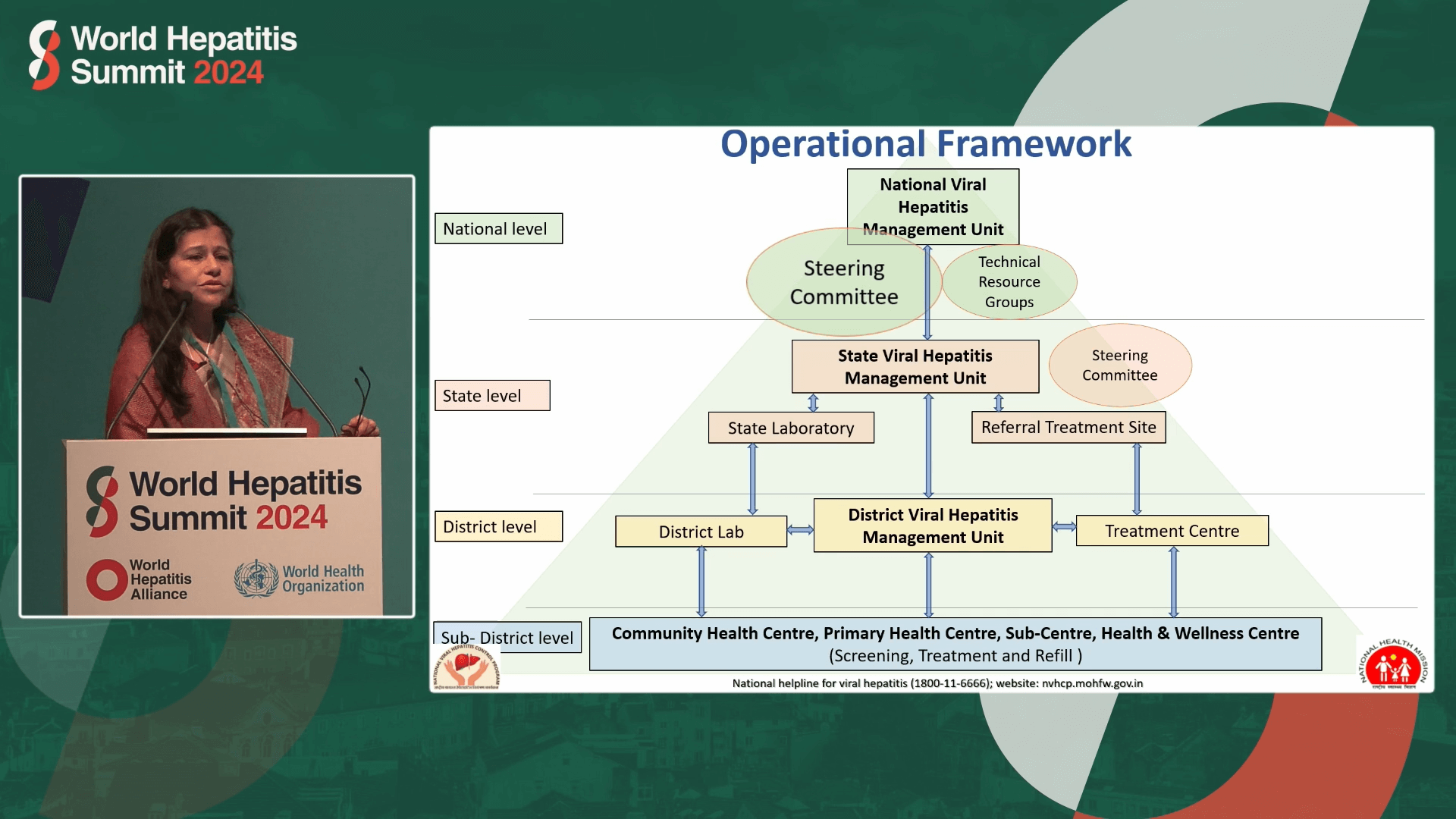
Given India’s complex system of governance with numerous states and districts, and the need to reach its immense population of 1.4 billion, the NVHCP adopted a strategy that relied heavily on integrating viral hepatitis services into the existing health infrastructure including administrative setups, buildings and staff.
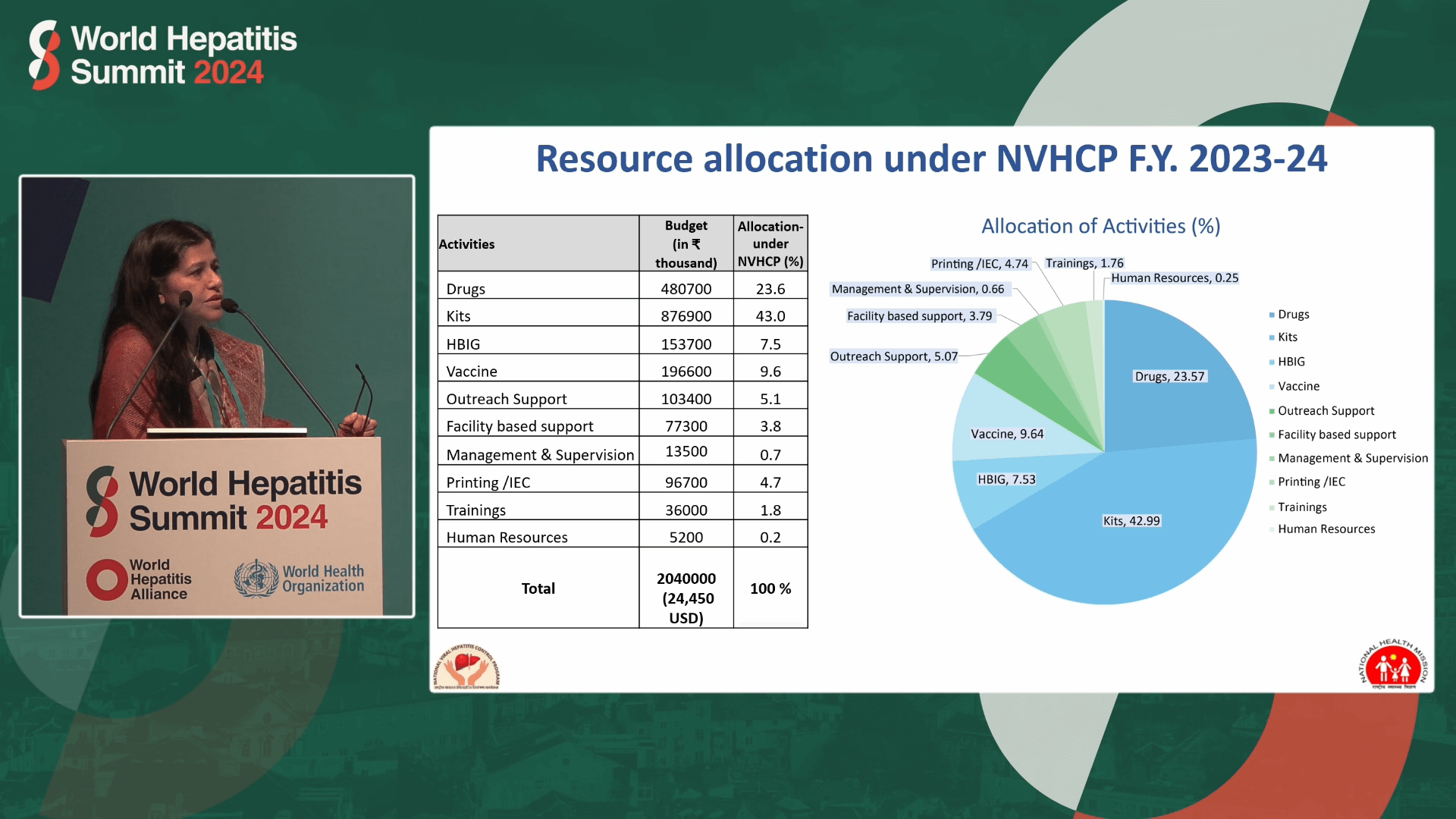
The integrated approach, said Dr Kabra, avoids duplication, allowing 100 per cent domestic funding and thus ensuring sustainability. National level operations include the overseeing of prevention, diagnosis and program management by the National Viral Hepatitis Management Unit, Steering Committee and Technical Resource Groups which liaise with corresponding states and districts level units which implement service delivery at community health centres, primary health centres, and wellness centres.
Integrating into existing screening services reduces double-handling, and maximises opportunities, getting “three tests done with one prick”
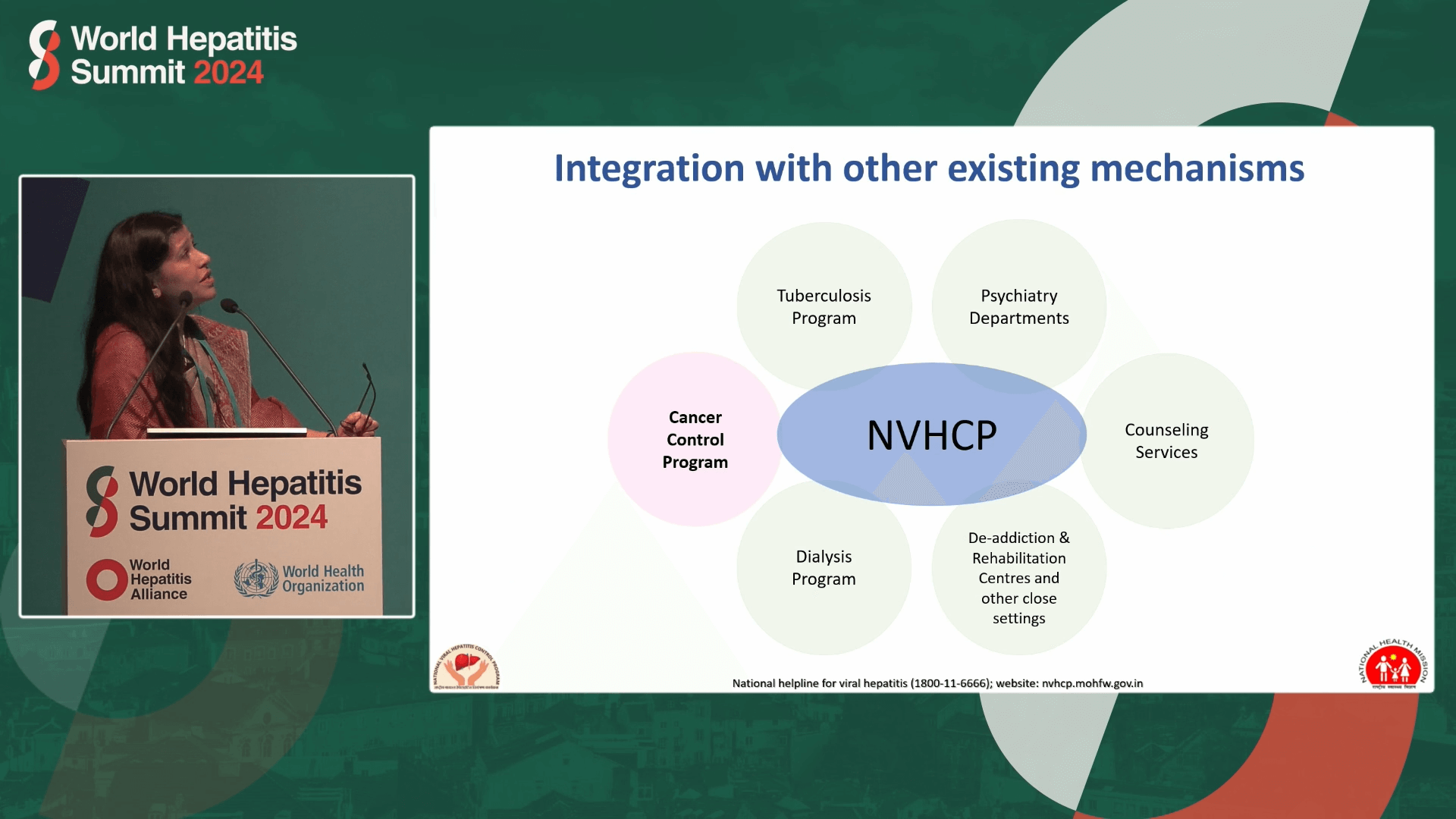
Integration with existing family health, drug and HIV services ensures access to priority groups such as pregnant women, newborns and people who use drugs. Other existing “mechanisms” include cancer control, tuberculosis, dialysis, blood transfusion and counselling programs.
Integrating into existing screening services reduces double-handling, and maximises opportunities, getting “three tests done with one prick”.
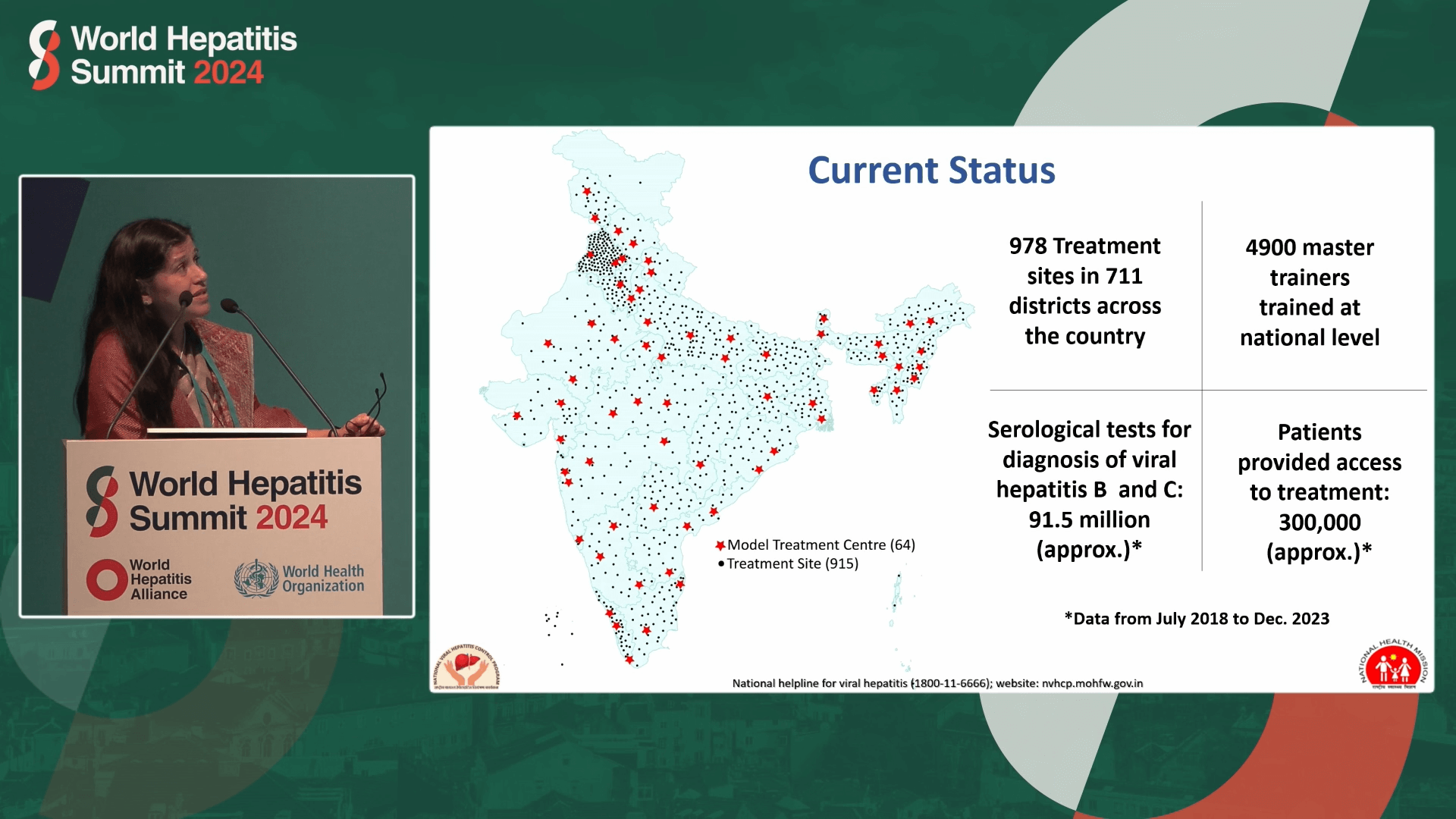
Between July 2018 and December 2023, the NVHCP carried out approximately 91.5 million hepatitis B and hepatitis C tests, with over 300,000 patients accessing treatment. There are 978 treatment sites in 711 districts across the country and 4,900 people trained who are able to go on to train others.
While the program has been successful, Dr Kabra said challenges remain. These include India’s vast geographical expanse and huge population, limited availability of finger prick test kits, lack of child-appropriate medications, and allocation of resources to states not always conforming to standard protocols prescribed by agencies.
Dr Kabra’s strong message was for countries which have an existing health system to not neglect that fact, to use the existing system instead of trying to build an entirely new “vertical” hepatitis program, and a “humble request” to agencies to align with local government protocols.


Last updated 4 September 2024
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates





