Global elimination of hepatitis C can only be achieved if innovative ways can be found for low- and middle- income countries to finance treatment so that it is affordable for the vast majority of people around the world living with the virus. This was the conclusion in a new study from the Kirby Institute.
Direct-acting antivirals (DAAs) have been a massively effective weapon in the fight to eliminate hepatitis C, with a cure rate of more than 95 per cent but access to these live-saving treatment is very dependent on where you live, the researchers found.
Almost 90 per cent of the 57 million people living with hepatitis C across the world are in low- and middle-income countries, and only half of these countries currently provide DAA treatments at an accessible cost, says the study, published in The Lancet Gastroenterology & Hepatology journal.
The research examined the registration, reimbursement and restrictions for hepatitis C treatments across 160 countries, representing approximately 95 per cent of the global population. There are between 190 and 200 countries in the world, depending on whose definition you use.
“Current direct-acting antiviral treatments [are] revolutionising the way we manage this condition. But there remains a high cost to the treatment in most countries, which has led to a disparate rollout globally, with many countries placing restrictions both on who can access it and who can prescribe it,” explained Dr Alison Marshall, who led the research at the Kirby Institute.
“Universal access to health coverage means all people should have access to the full range of quality services they need, irrespective of who they are, where they are born, or the nature of their health condition.”
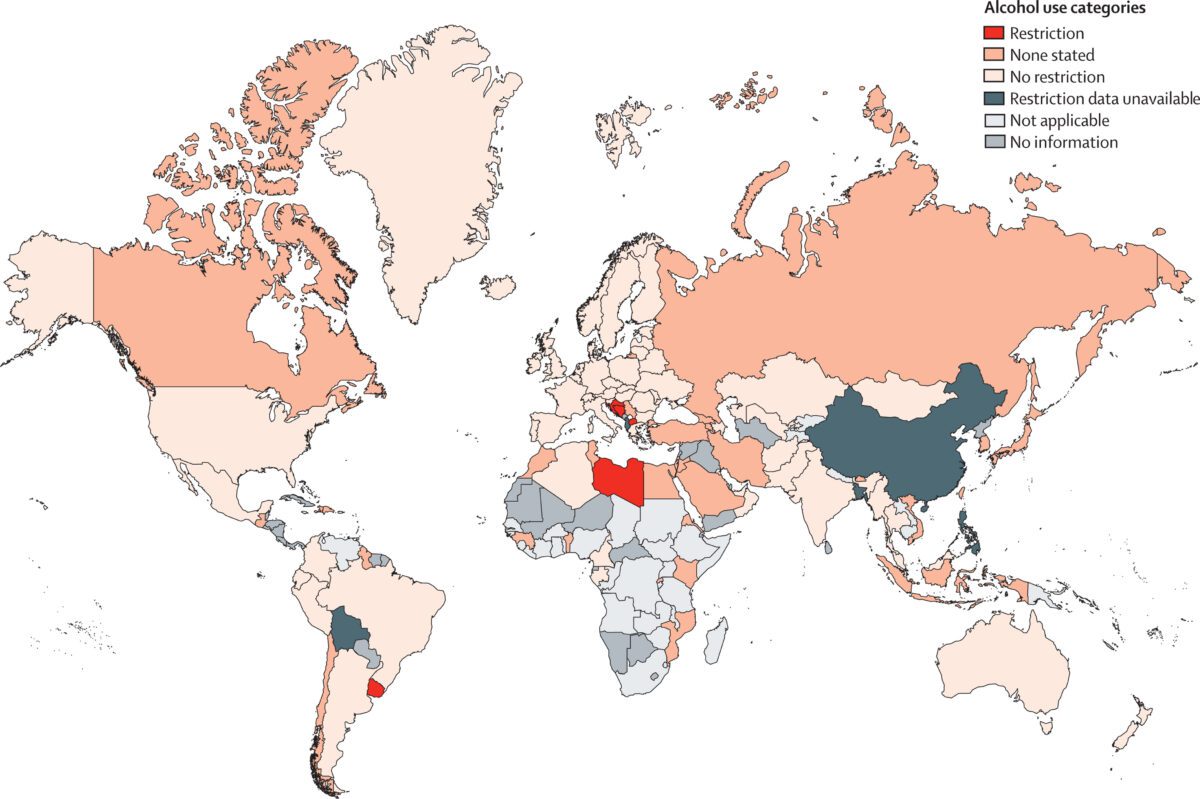
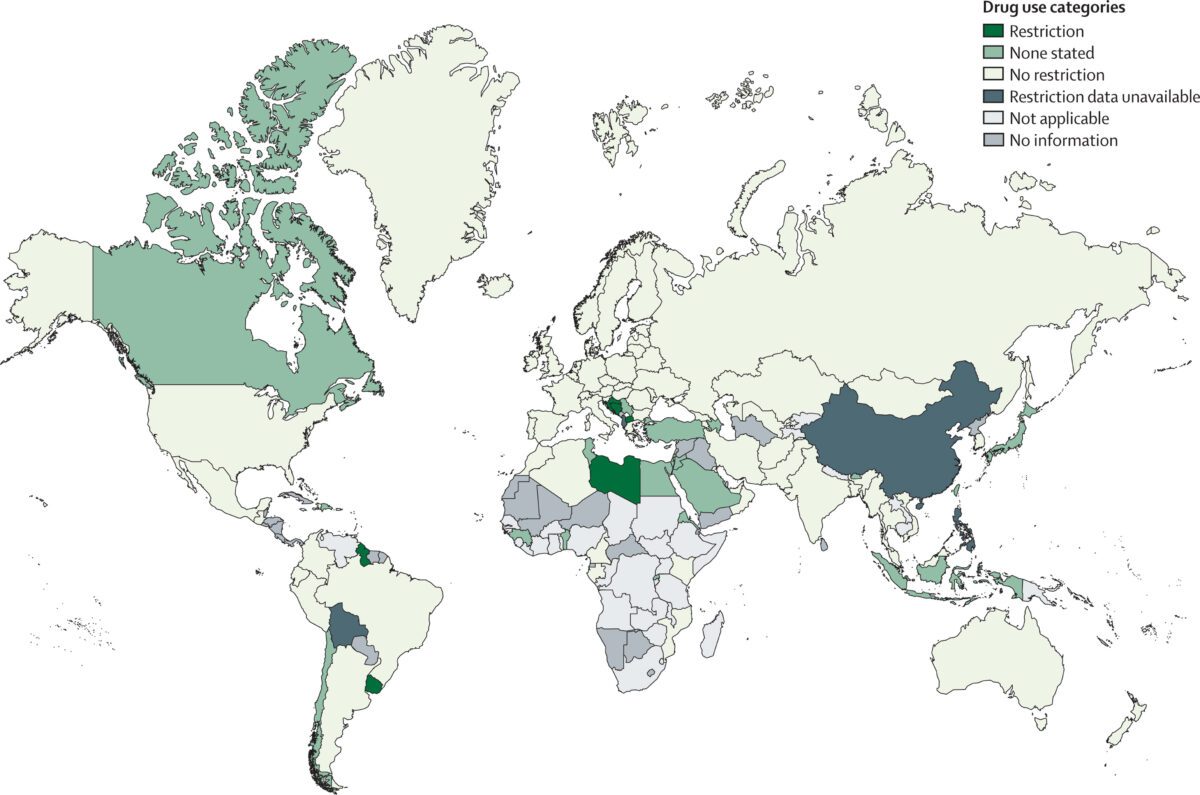
According to the research, of the 160 countries analysed, 91 per cent have at least one hepatitis C treatment registered, but only two thirds of countries provide their residents with access to reimbursed (subsidised) treatment, in the way that Australians can access DAAs through the Pharmaceutical Benefits Scheme (PBS) at minimal cost. Among low- and middle-income countries, just over half provide reimbursement. Seven countries restrict access based on drug use and five based on alcohol use, something for which there is no good reason in terms of treatment efficacy.
“Given that the majority of people living with hepatitis C live in low- and middle-income countries, we need to see much higher numbers of countries providing reimbursement for hepatitis C therapies, especially if we are to meet the World Health Organization target to eliminate hepatitis C as a public health threat by 2030,” Dr Marshall said. “Most people living with hepatitis C globally are marginalised and face multiple challenges to accessing care. If cost is a barrier to seeking cure, they are unlikely to seek treatment, which poses risks for their health, as well as for onward transmission.”
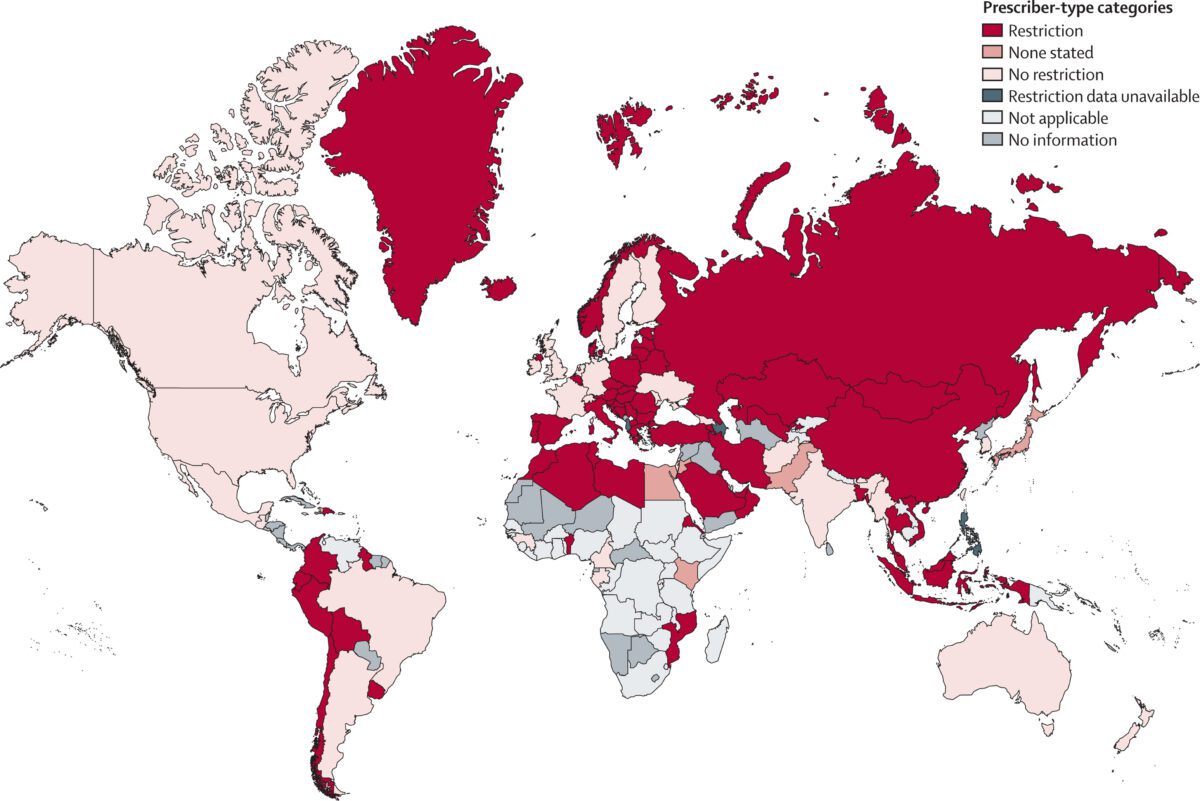
Another barrier to accessing DAAs is who can prescribe the medications. The analysis found that in 61 per cent of countries, a specialist (e.g., a liver disease specialist or infectious disease specialist) was required to prescribe the medication. This restriction reduces the proportion of available prescribers and most often requires patients to receive treatment from a specialist centre, often hospital-based.
…need for more innovative financing models to encourage and facilitate increased access to treatment…
“This is a major barrier for marginalised population groups such as people who use or inject drugs – people who are more likely to experience stigma in healthcare settings and avoid attending hospital-based centres. Increasing task sharing of hepatitis C testing and treatment to non-specialised centres such as primary care centres would broaden access,” explained Professor Jason Grebely, head of the Hepatitis C and Drug Use Group in the Viral Hepatitis Clinical Research Program at the Kirby Institute, and senior author on the paper.
The researchers conclude that there is a need for more innovative financing models to encourage and facilitate increased access to treatment, especially in low- and middle-income countries.
“There have been some great initiatives, such as the Clinton Health Access Initiative, and The Hepatitis Fund who have helped to facilitate price agreements with generic manufacturers to provide treatments to low- and middle-income countries for $US60 per treatment course, but we need to do more to assist countries to increase access to these lifesaving treatments,” said Professor Grebely.
This is vitally important. Consider Egypt, a country that until 10 years ago had one of the world’s highest rate of hepatitis C, and where the average weekly wage is equivalent to less than AU$50. Most people under this financial pressure simply do not have the money to spare to pay for medical treatment unless it is massively subsidised or even free. So the Egyptian government provided free HCV testing and treatment for the population, and now Egypt has one of the world’s lowest HCV rates, and is the first to achieve WHO validation on the path to elimination of hepatitis C.
Chief Executive Officer of the World Hepatitis Alliance, Rachel Halford, says the research is both alarming and timely.
“We hope this research will motivate action from policymakers and healthcare professionals globally, as the urgency to tackle hepatitis cannot be overemphasised.
“Eliminating viral hepatitis will prevent hundreds of thousands of lives lost to liver cancer and other liver diseases resulting from chronic hepatitis. As a global hepatitis community, we must collaborate to drive change. We commend the Kirby Institute’s contribution to this global collaboration with this research.”
Last updated 10 April 2024
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates





