Sydney-based researchers have discovered a new way to treat hepatocellular carcinoma (HCC), the most common type of liver cancer, and the third leading cause of cancer death worldwide. Hepatocellular carcinomas are often caused by late-stage hepatitis, and since they often show no outward symptoms, they are often diagnosed late and hard to treat effectively in time. Though the new treatment has only been trialled in mice, it is hoped to move on to human trials soon.
The study, led by the Centenary Institute, a New South Wales-based research organisation focused on treatments for serious illness, revealed an encouraging treatment strategy involving the use of a new drug called Blockmir CD5-2.
In the trials, Blockmir was combined with a drug called ‘programmed cell death protein 1 antibody’ (anti-PD1 antibody). Cancer is what happens when cells start evading the normal process of death and renewal which is built into their DNA. This antibody helps counteract that evasion. This combination of two medications proved effective in reducing liver tumour size in mice. The research was published in the journal Frontiers in Immunology.
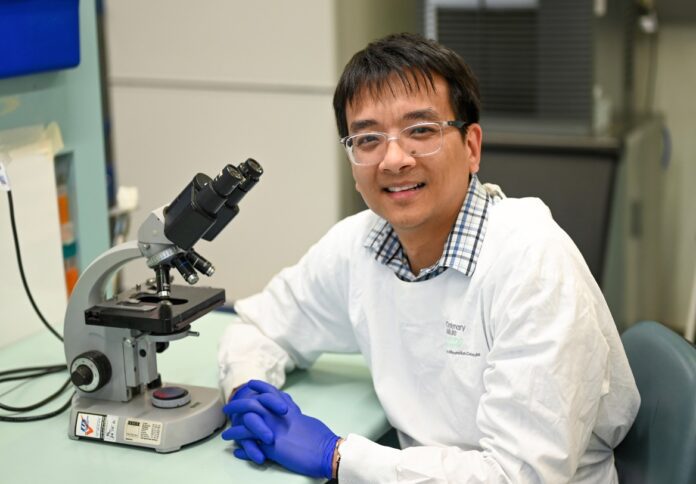
Lead author of the study, Dr. Ken Liu, a researcher in the Centenary Institute’s Centre for Cancer Innovations, said in a media statement that the discovery was exciting and had the potential to be a viable treatment for advanced liver cancer.
“The synergistic effect of the drugs Blockmir CD5-2 and anti-PD1 antibody significantly reduced the size of liver tumours in mice in our study. We believe that this dual-drug approach enhances the immune system, rendering it more efficient in combating cancer cells and reducing tumours,” said Dr. Liu.
Dr. Liu explained that liver tumours often have abnormal blood vessels and low oxygen levels, creating an environment that suppresses the immune system and the body’s ability to fight cancer.
“Blockmir CD5-2 addresses this issue by promoting the health of tumour blood vessels through the activation of a protein called VE-Cadherin. This results in improved blood supply and oxygen levels within the tumours,” said Dr. Liu.
“The enhanced blood vessel conditions within the tumours means that more cancer-targeting immune cells, specifically cytotoxic T cells, can infiltrate the tumour and effectively combat the disease,” he said.
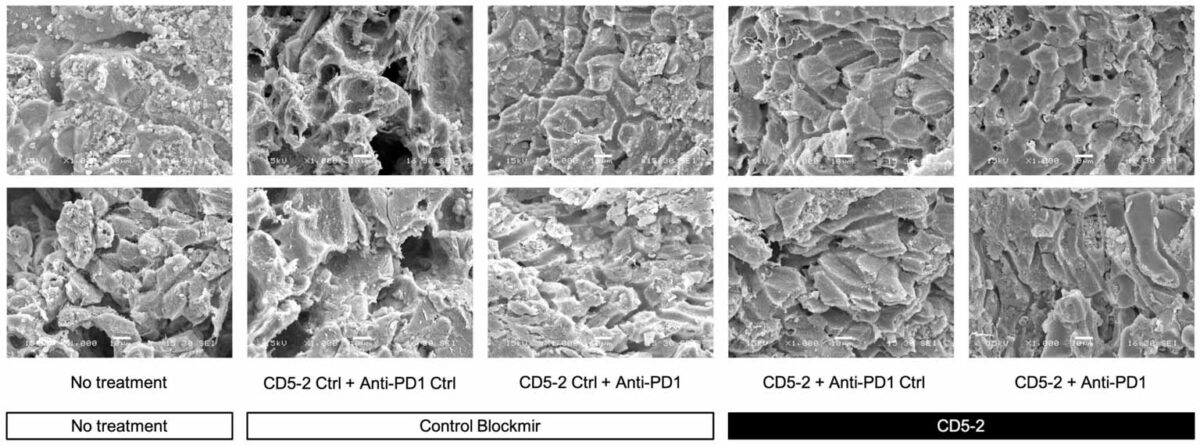
The researchers said that use of the anti-PD1 antibody was also a crucial component of the innovative treatment approach, helping the immune system fight cancer more effectively by blocking a protein that hinders the immune response.
Senior study authors Professor Jennifer Gamble (from the Centenary Institute’s Centre for Healthy Aging) and Professor Geoff McCaughan (from the Centenary Institute’s Centre for Cancer Innovations) said that current effective treatment options for liver cancer were limited and that the new therapeutic approach held tremendous potential for effectively treating such a challenging disease.
The next stage will be to trial this approach in humans. If it works similarly well there, it will be an invaluable weapon in the fight against a difficult and dangerous disease.
Last updated 16 May 2024
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates