Clean needle program tops the list of strategies outlined in a consensus statement released by the Harm Reduction in Prisons Working Group. The statement aims to provide a clear, concise overview of evidence-based harm reduction interventions needed to reduce injecting-related harms in Australian prisons.
Briefly, the proposed interventions are:
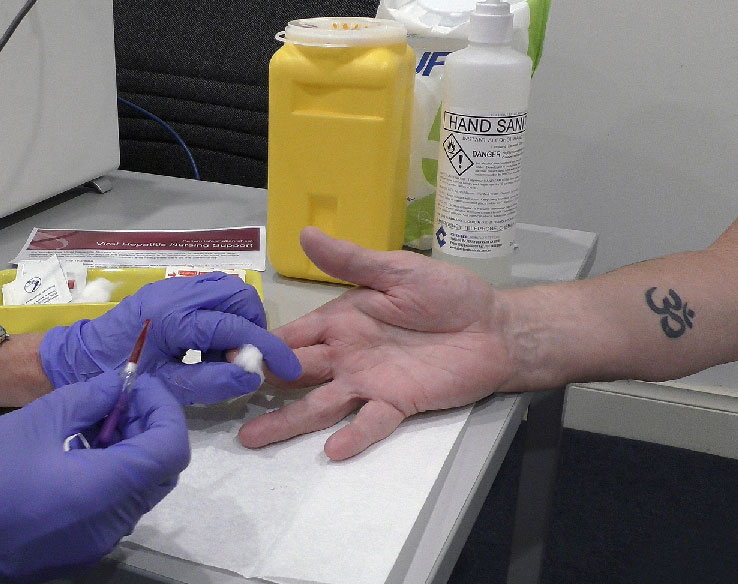
Regulated provision of sterile injecting equipment to people who inject drugs – commonly known as Needle and Syringe Programs (NSP) or Clean Needle Programs (CNP). Evidence show that CNPs work to reduce blood-borne virus transmission and is considered best practice with evidence from 10 countries showing they work just as well in prisons as they do in the community.
The statement pointed out that the lack of regulated access to sterile injecting equipment is associated with new blood-borne virus infections and reinfections among prison populations despite the provision of direct-acting antivirals. Regulating access to new sterile needles is also an important strategy in preventing injecting-related injuries and disease and thrombophlebitis.

Overdose prevention sites that provide a safer place for people to inject drugs under the supervision of health professionals where overdose can be quickly reversed. They provide opportunities for contact and referral to other services. Evidence show they reduce the risk of overdose and improve access to care.
Needle cleaning agents – Bleach is an effective agent against the hepatitis C virus and HIV when it can be used properly to clean needles and syringes. Where people in prisons cannot access clean and sterile injecting equipment, needle cleaning agents should be provided.
Naloxone – Evidence shows that take-home naloxone programs which train participants to recognise overdose and administer the opioid reversal drug, reduces overdose deaths both in prison and in the high-risk period following release from prison.
Peer-led education and programs – Peer educators a more credible and trusted source of information for people in prison. Extensive research shows that education programs in prison are more effective at reducing risky behaviours when developed and delivered by peers. Peer support programs and peer workers provide emotional support and practical information, such as supporting engagement in testing.
Opioid Agonist Treatment (OAT) is a cost-effective treatment that is associated with reductions in harmful drug use, blood-borne infections and death, both in the community and in prison (56-58). OAT has also been found to improve prison safety and reduced rates of re-offending among people in prison (3). Combined use of OAT with needle syringe programs is more effective at preventing new blood-borne virus infections than just providing OAT alone.
Blood-borne virus (BBV) screening should be offered to everyone entering prison and then yearly and be voluntary. International research suggests that opt-out systems where screening is standard practice for everyone rather than opt-in, is best for maximum take-up of screening, as long as people are adequately informed of their right to refuse.
Hepatitis B virus (HBV) vaccination of all people in prison is recommended by the Australian government. HBV immunisation reduces the pool of people infected with HBV thereby reducing the likelihood of transmission.
Hepatitis C virus (HCV) treatment – Direct Acting Antivirals (DAAs) are an approved medication that have special prescribing status so can be accessed by people in prison under Medicare. The provision of unrestricted access to DAAs has cured nearly half of all people living with hepatitis C in Australia (from 2016 to 2020) and has reduced incidence of new hepatitis C infections in Australia.
However, DAA treatment is less effective as prevention strategy in situations where there are high rates of risky injecting behaviour and other harm reduction is unavailable. It needs to be combined with effective primary preventative measures such as needle exchange programs to achieve hepatitis C elimination.
HIV prevention and treatment – Pre-Exposure Prophylaxis (PrEP) is a medication that prevents HIV acquisition and Post-Exposure Prophylaxis (PEP) is a course of medication that can be taken after potential exposure to HIV to prevent acquisition. Antiretroviral Therapy (ART) is an approved medication to treat HIV. PrEP, PEP and ARTs are funded on the Pharmaceutical Benefits Scheme.
The Working Group in its statement said the recommended interventions have application for all people at risk of injecting-related harm, disease and death in prisons and hoped that the statement would assist policy makers at all levels of government in all jurisdictions to apply a broader lens to harm reduction and to understand why a comprehensive response is needed.
Last updated 15 May 2024
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates