While only 2.3 per cent of South Australia’s population is Indigenous, almost a quarter (22 per cent) of people in the State’s prison system are Aboriginal. The prison population is also rife with blood-borne viruses, including hepatitis B and C—viruses which also disproportionately affect Indigenous people in the general population.
Untreated chronic health conditions (as well as hepatitis these commonly include mental illness, diabetes, heart and respiratory diseases, cancer and drug use), compounded by a prisoner’s isolation from their family and community, and a fracturing in their cultural identity and spiritual well-being, can be catastrophic for an Aboriginal person in the prison system.
This means that it is critical that access to good healthcare be a priority. And the only way in which that can succeed is in partnership with South Australia’s Aboriginal community and Aboriginal-specific health services.
SA Health, in particular SA Prison Health and Watto Purrunna (the Aboriginal Primary Care Services for Northern Adelaide LHN), had been seeking an evidence-based model of care specific to the health needs of adult Aboriginal prisoners. It was quickly established that not much existed, so Wardliparingga, the Aboriginal Health Research Unit at the South Australian Health and Medical Research Institute (SAHMRI), was approached to assist in designing an evidence-based model of care.
The engagement of Wardliparingga was a decisive move to acknowledge that Aboriginal research is done best when in the hands of Aboriginal people, and this research is vital: it can save lives.
“The objective of this research was challenging for us, and we had to discuss many of the complex health needs of our community,” explain Heather Agius and Evelyn Varcoe, representatives of the Adelaide Grannies Group, a peer support network of Aboriginal grandparents who advocate on behalf of issues affecting their children, grandchildren and their community. “By exploring different stakeholders’ points of view, and by sharing what kind of ‘model of care’ we could design to address the broad needs of Aboriginal adult prisoners, we highlighted the need for qualitative research that would give us the opportunity to inform policy and practice.
“Our Elders hope that this resulting model of care will be taken seriously by governments, and that stakeholders will make it their business to participate and implement changes, for the betterment of our Aboriginal adult and youth prisoners in South Australia.”
On the first Monday in February, the new Model of Care for Aboriginal Prisoner Health and Wellbeing for South Australia report was launched.
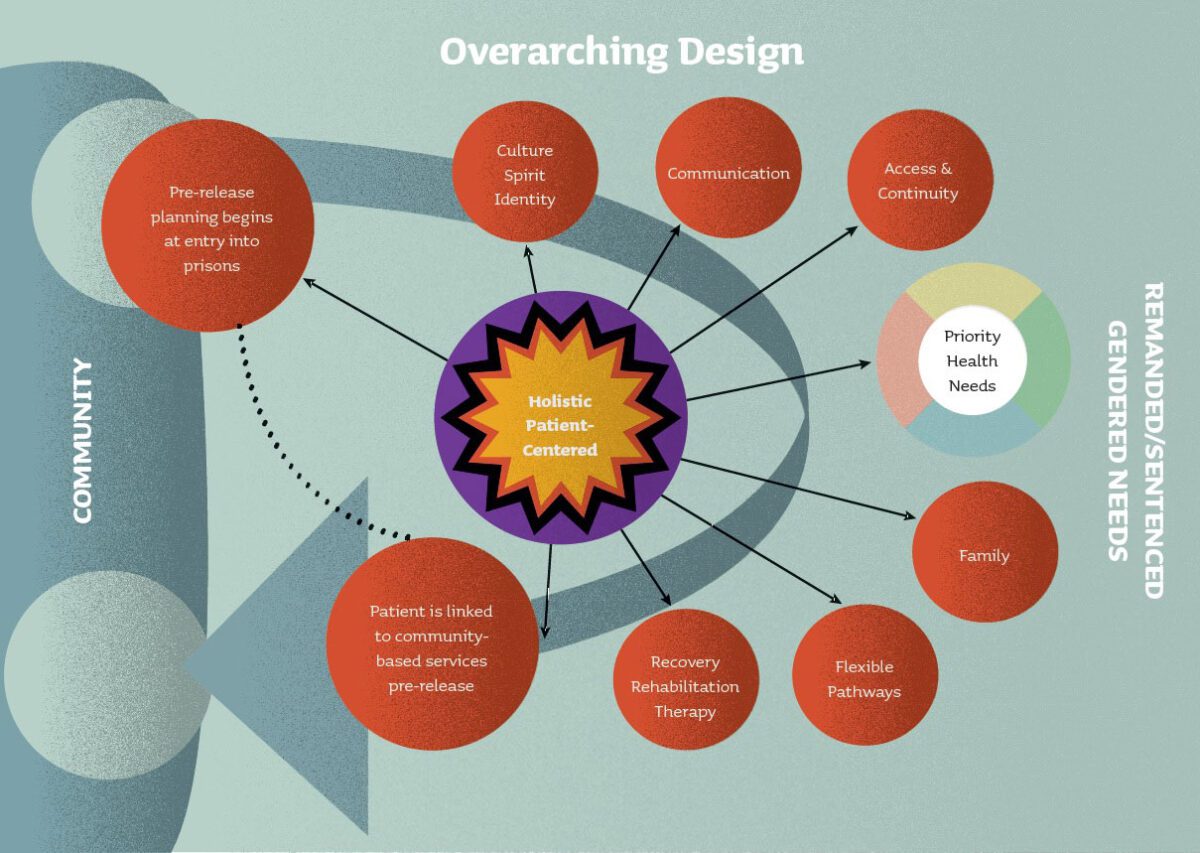
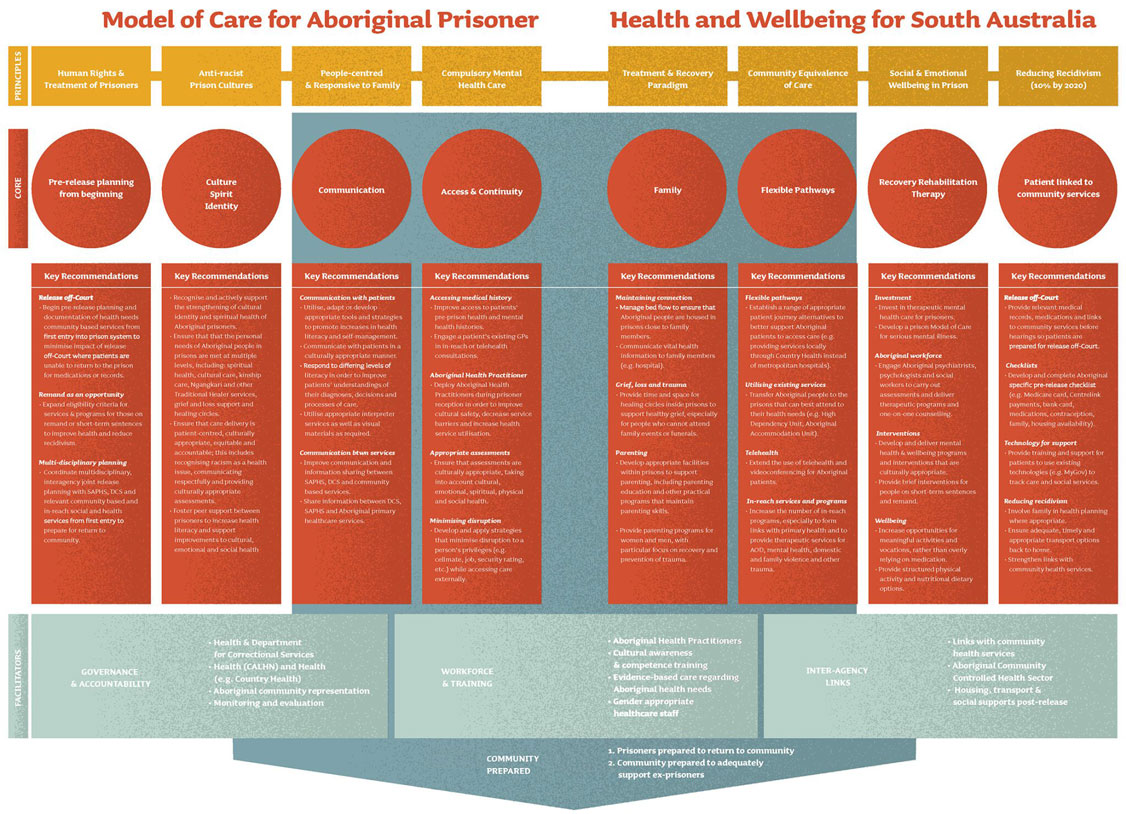
The Model of Care emphasises that Aboriginal prisoners are members of communities both inside and outside of prison, and that their release into the wider community at the completion of their sentences needs more consideration. It notes the unique needs of remanded and sentenced prisoners, and differing needs by gender. The model has eight core elements:
- pre-release planning begins at entry to prison
- culture, spirt and identity
- communication
- access and continuity
- family
- flexible pathways
- recovery, rehabilitation, therapy
- prisoners need to be linked to community-based services pre-release
For more details on each element, click on the chart below to enlarge the details.
SA Health has acknowledged the challenges to the Model of Care’s implementation, but has enthusiastically endorsed it for implementation.
One sour note is that the release of this Model of Care report has been met with total apathy from the media and this article is, at the time of writing, the only publicity it has received online. We hope that this will change and that the Model of Care will be a success.
You can download the report or its executive summary from SAHMRI.
Last updated 10 April 2025
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates