One of the key planks of Australia’s hepatitis C elimination strategy is increasing treatment through management by General Practitioners (GPs), making it easier for individuals to receive treatment and facilitating access to hard-to-reach communities.
GP training programs have been rolled out across the country and GP prescribing had increased from eight per cent in March to 31 per cent in December. However, most prescribing (62 per cent) are still by specialists and GP prescriptions in South Australia, Northern Territory, ACT and Victoria are significantly below average.
For GPs who deal with a host of ailments and don’t see many patients with hepatitis C, lack of familiarity with treatment guidelines and specialist support pathways are barriers to prescribing.
A survey of GPs by the Royal Australian College of General Practice (RACGP) identified a need to develop “user-friendly, ‘in-consultation’ pathways for GPs not experienced in the treatment of HCV”.
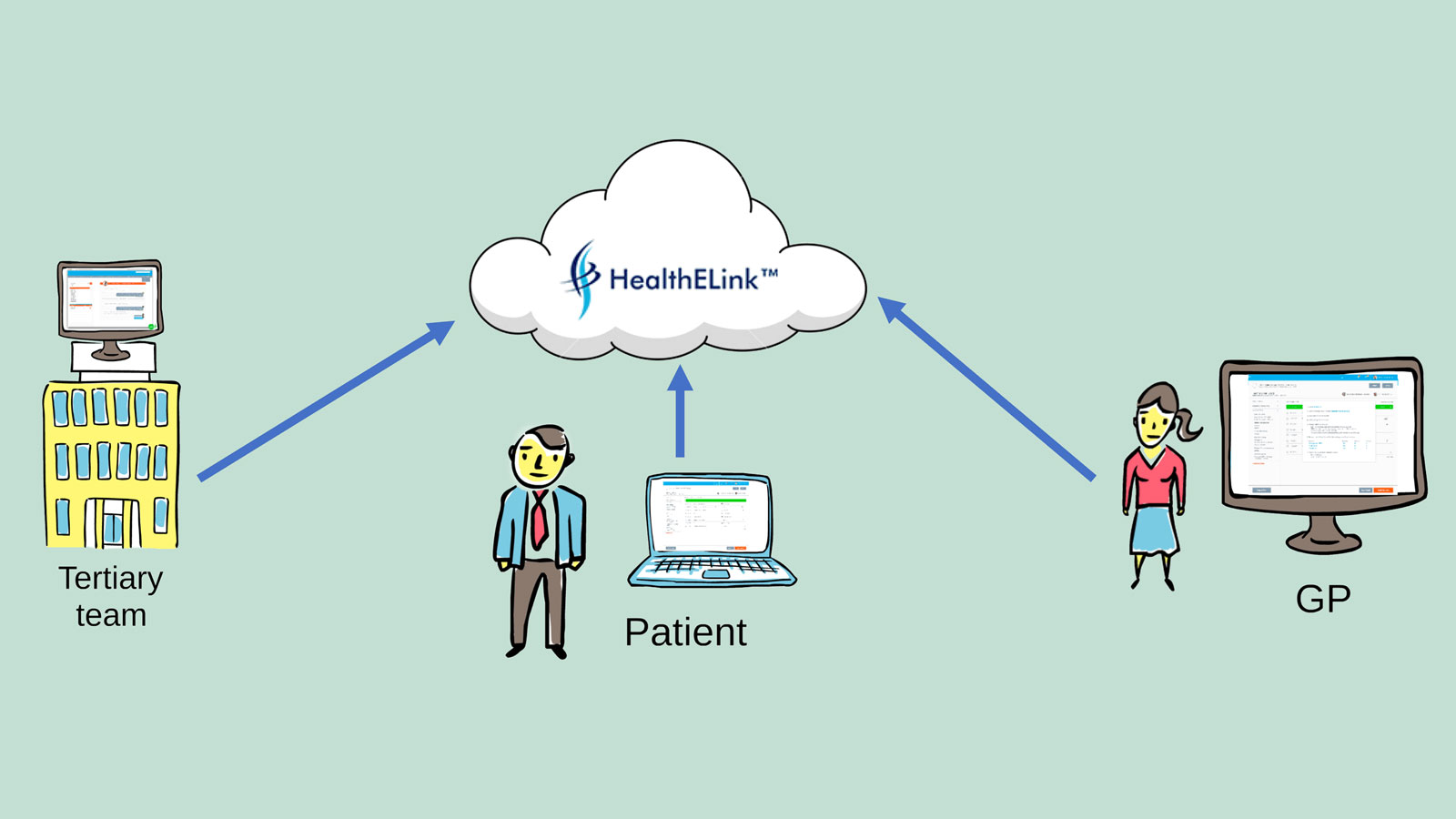
HealthELink is a web-based platform developed by doctors for doctors in response to this need. The online tool connects the GP, specialist, hepatitis nurse and patient together facilitating communication and decision-making in the treating hepatitis C.
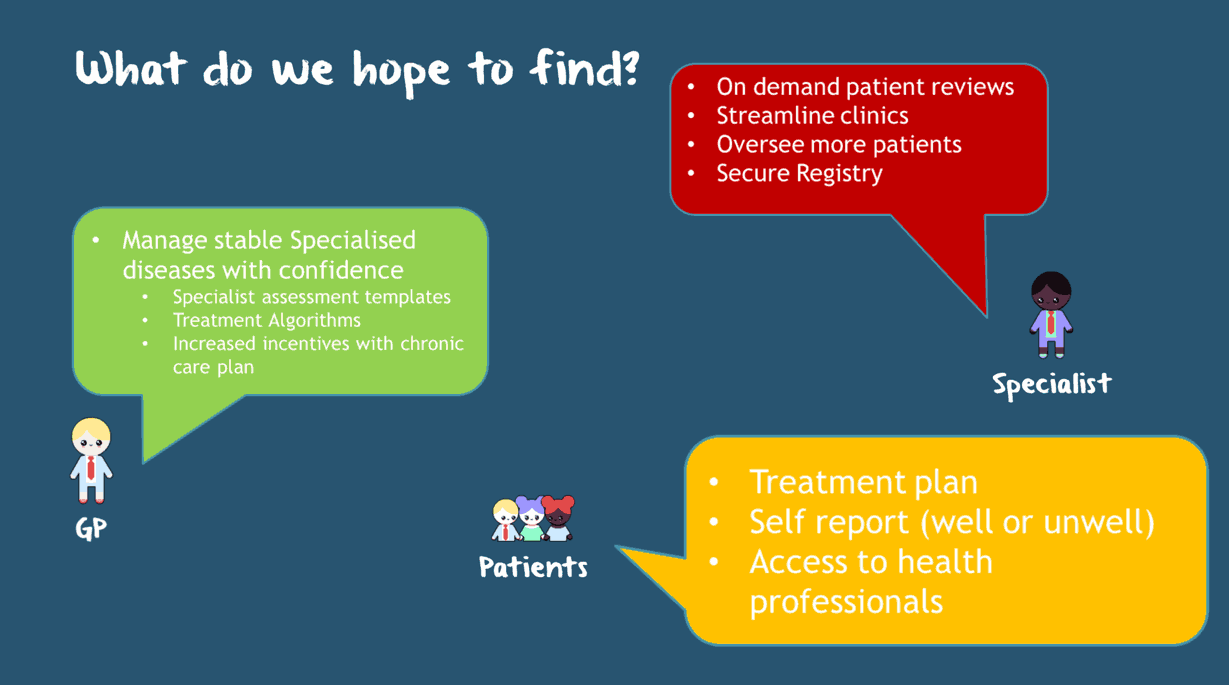
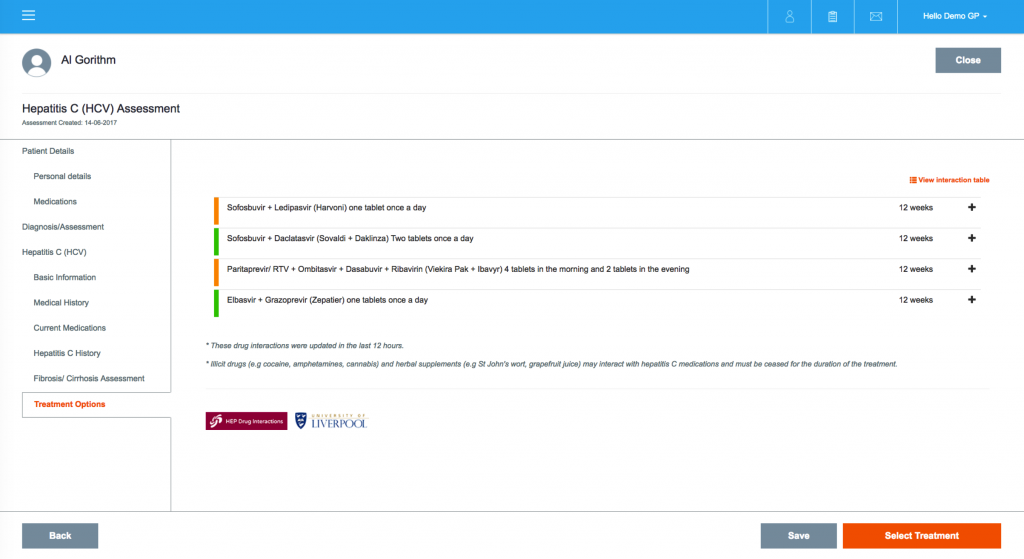
GPs can electronically refer to a specialist to review and approve hepatitis C treatment plans which are automatically generated based on current Australian hepatitis C treatment guidelines, including interpretation of fibrosis markers and assessment of medication interactions.
HealthELink provides secure messaging between GPs, specialists and nurses and patients can login and view their treatment plan, mark tasks as complete and message their viral hepatitis nurse.
HealthELink is currently recruiting GPs for a multi-centre trial involving tertiary hospitals and referring GPs in the Northern Territory, South Australia and Victoria.
Dr Eddie Tse, a principal investigator in the project, said the development of HealthELink is currently funded by four doctors with support from government (business innovative) and non government grants.
“We are also engaging the department of health and pharmaceutical companies for support to further develop and refine the platform, but it is with the understanding that they will no way interfere with the treatment algorithm which is based on national (ALA) guidelines,” he said.
“There will be no advertising from these companies on the platform.
Dr Tse, who is Head of Clinical Hepatology at the Royal Adelaide Hospital, said the online tool will be available free of charge to users including doctors, patients and other health professionals.
“The purpose of the HealthELink project at the moment is proof of concept, to determine if a web-based shared care model for chronic disease is feasible. Currently, there are no plans for commercialization,” he added.
“Should we prove that this is successful, we hope to source funding with our proof of concept data to allow GPs as well as viral hep nurses alike, to use it for free.
“Unfortunately, HealthELink will require funding to keep running covering costs of hosting, support and so on. We hope that it will eventually come from the Federal government.
“Other sources of funding we are looking into include departments of health, Primary Health Networks, hospitals and pharmaceutical companies.”
HealthELink project coordinator, Dr James Haridy recently received a national digital health award for his work on the system. To register, see a preview or find out more, visit HealthElLink Study.
Last updated 1 June 2024
More from:
Enjoyed this article? Subscribe to be notified whenever we publish new stories.
Subscribe for Updates