Aaron* was shocked when his hepatitis C rapid test came back positive. When he was approached by a nurse and peer worker at the Hutt Street Centre to get tested, he had been pretty sure his results would be ok.
If you’re homeless and have no symptoms, testing for hep C is probably low on the list of priorities. Aaron considered himself pretty clued in about blood-borne virus risk; he’d been injecting drugs for many years and was an expert in technique, always using clean equipment.
He was keen to go on treatment straight away and was indeed referred immediately to get started.
Viral Hepatitis Nurse, Lucy Ralton said Aaron later told her that he had seen his GP due to persistent fatigue but hadn’t been screened for an HCV infection at the time. “He was very glad he got talked into having a test that day and said he only did so because he was asked,” she said.
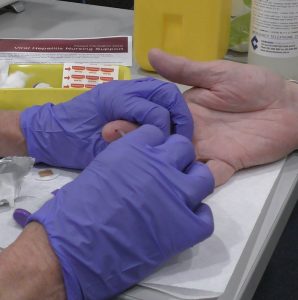
The testing clinic at the Hutt Street Centre was part of the PROMPt study where a nurse and a Hepatitis SA peer worker together and directly approach individuals to invite them to have a test. Anyone with a positive result was referred to the community Viral Hepatitis Nurses for treatment.
What programs like this has shown is the importance of connections and support for community and health workers who provide services to clients who are homeless and at risk of hepatitis C.

Rates of hepatitis C prevalence are higher in people who are homeless compared to the general population. Studies, including a recent South Australian study, have found that frequent injecting drug use and hepatitis C prevalence are associated with homelessness.
Knowing that they can contact a local organisation … and get all the information they need … will empower them to … be part of the effort to eliminate hepatitis C…
Despite this, Nurse Ralton said, many of those working with people who are homeless may not be aware of how easy and effective hepatitis C treatment is or of the benefits to the client and where to turn for information and support.
“Health workers often have key relationships with clients who are homeless and at risk of hepatitis C. They are ideally placed to encourage individuals to get tested and to support them during treatment.
“Knowing that they can contact a local organisation such as Hepatitis SA and get all the information they need including local specialist service contact details will empower them to see that they can be part of the effort to eliminate hepatitis C and improve the health of their clients.”
She explained that there is a clear association between homelessness and hepatitis C risk factors such as injecting drug use. “Given the overlap between homelessness and injecting drug use, homelessness services will inevitably find that many of their clients have or are at risk of acquiring hepatitis C and they may not know what to do,” she said.
“Studies have found that people who are homeless face many barriers to hepatitis C testing and treatment including not knowing what support exists, incarceration, ineffective healthcare communication methods (including the referral process and telephone coordination) and difficulty keeping appointments.
“Drug misuse is a factor that can lead to homelessness, however homelessness can also cause drug misuse or worsen an existing problem.
“Scaling up hepatitis C prevention, screening and treatment to address hepatitis C transmission among the homeless within existing community-based services and primary care is a priority if Australia is to realise the goal of eliminating hepatitis C by 2030.”
One way to improve access to hepatitis C care for this vulnerable group, is to bring together different services to explore ways of working together to make the process as simple as possible for both service providers and clients.
New models of care that integrate peers and healthcare workers have demonstrated that community-based screening, point of care testing and on the spot prescribing by either a nurse practitioner or GP in a non-judgmental and friendly environment can improve screening and treatment uptake. PROMPt – the project which helped Aaron get cured of his hepatitis C – was one example of such a model.
C the Whole Story was an online forum hosted by ASHM to discuss this challenge to provide participants with the tools, contacts and confidence to be able to discuss HCV screening and treatment with their clients, as well as create the opportunity for people to connect and explore ways for services to work together. To enquire about forum recordings or similar upcoming events, contact ASHM at ashm@ashm.org.au.
*Name changed to protect privacy
